High Hopes, Murky Data: How One Cannabis Heart Study Got Twisted in Translation
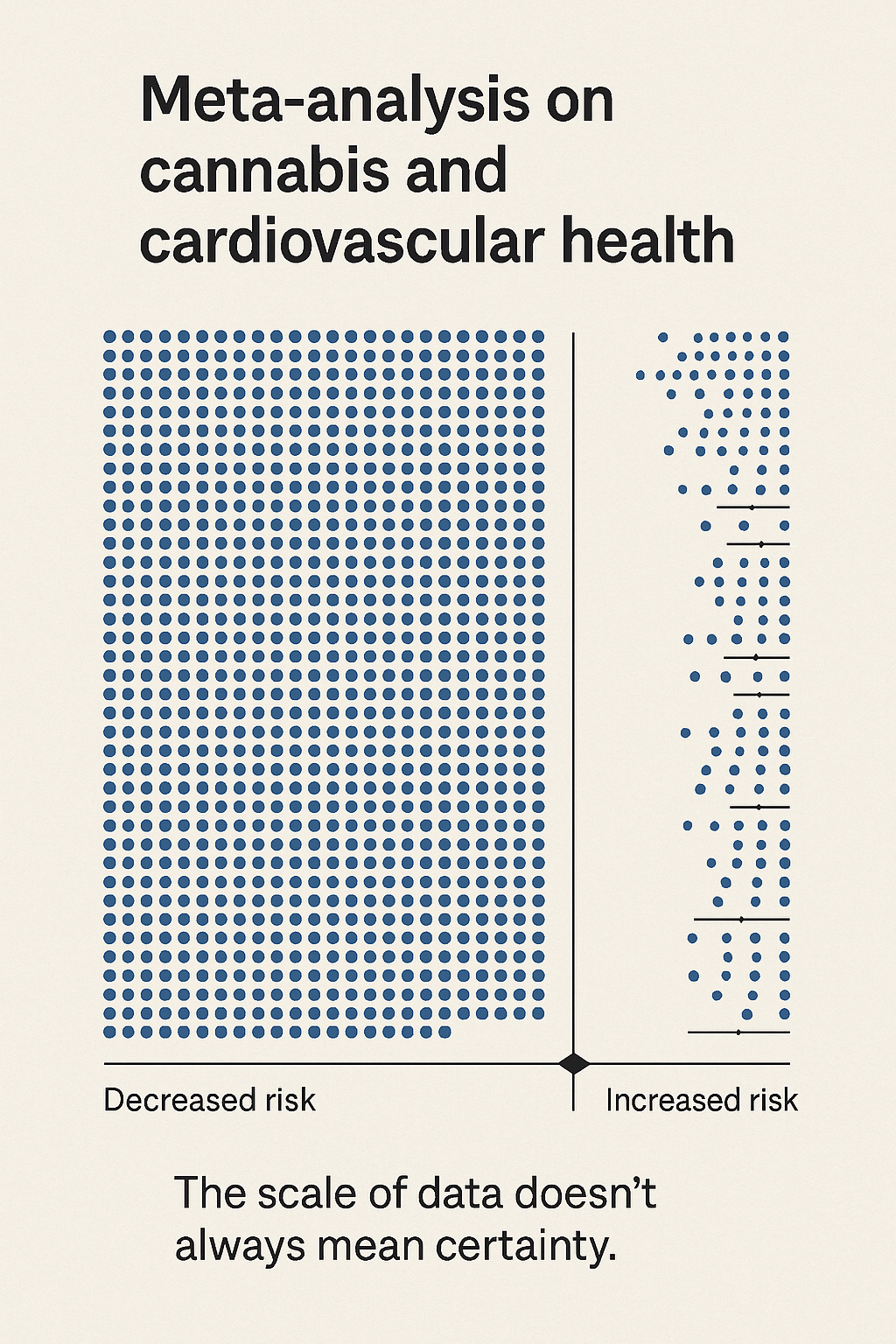
A massive meta-analysis. Millions of patients. And still… more questions than answers.
The meta-analysis making waves across the NYTimes, CNN, and Fox tried to build a mountain out of a molehill—only to realize too late it was standing on statistical quicksand.” 🏔️🫠
This post unpacks a recent publication titled “Cardiovascular risk associated with the use of cannabis and cannabinoids: a systematic review and meta-analysis” by Wilhelm Storck, Meyer Elbaz, Cécile Vindis, Amélia Déguilhem, Maryse Lapeyre-Mestre, and Emilie Jouanjus. The authors attempted to draw connections between cannabis use and heart-related events by pooling observational data from around the world. But as we’ll explore, their conclusions raise more questions than certainties—and may be built more on assumptions than airtight science.
🍃 The Perils of Big Claims in Blurry Studies
This week, when you scan headlines like “Cannabis May Harm Your Heart,” your pulse might quicken—for reasons having little to do with science. Especially if you’re one of the tens of millions using cannabis for stress, sleep, or pain, or if you’ve had a front-row seat to how quickly misinformation about this plant spreads like wildfire across the media landscape.
But this time, the headline isn't just hype—it’s based on a new meta-analysis that pooled data from over 400 million people.
So… should we panic?
Let’s pause before clutching our chests. Because while the dataset is enormous, the actual findings are far less dramatic than the framing suggests. In fact, once you crack open the details, what emerges isn’t a definitive indictment of cannabis—it’s a study more defined by what it can’t say than what it can.
What are we really looking at here? A red flag? A ripple? A Rorschach test?
Grab a seat. And a CBD chill pill. Let’s unpack it together.
(Have a take? Think this study was spot on—or way off? Leave a comment below ⬇️.)
🧠 Part 1: Association ≠ Causation (Still.)
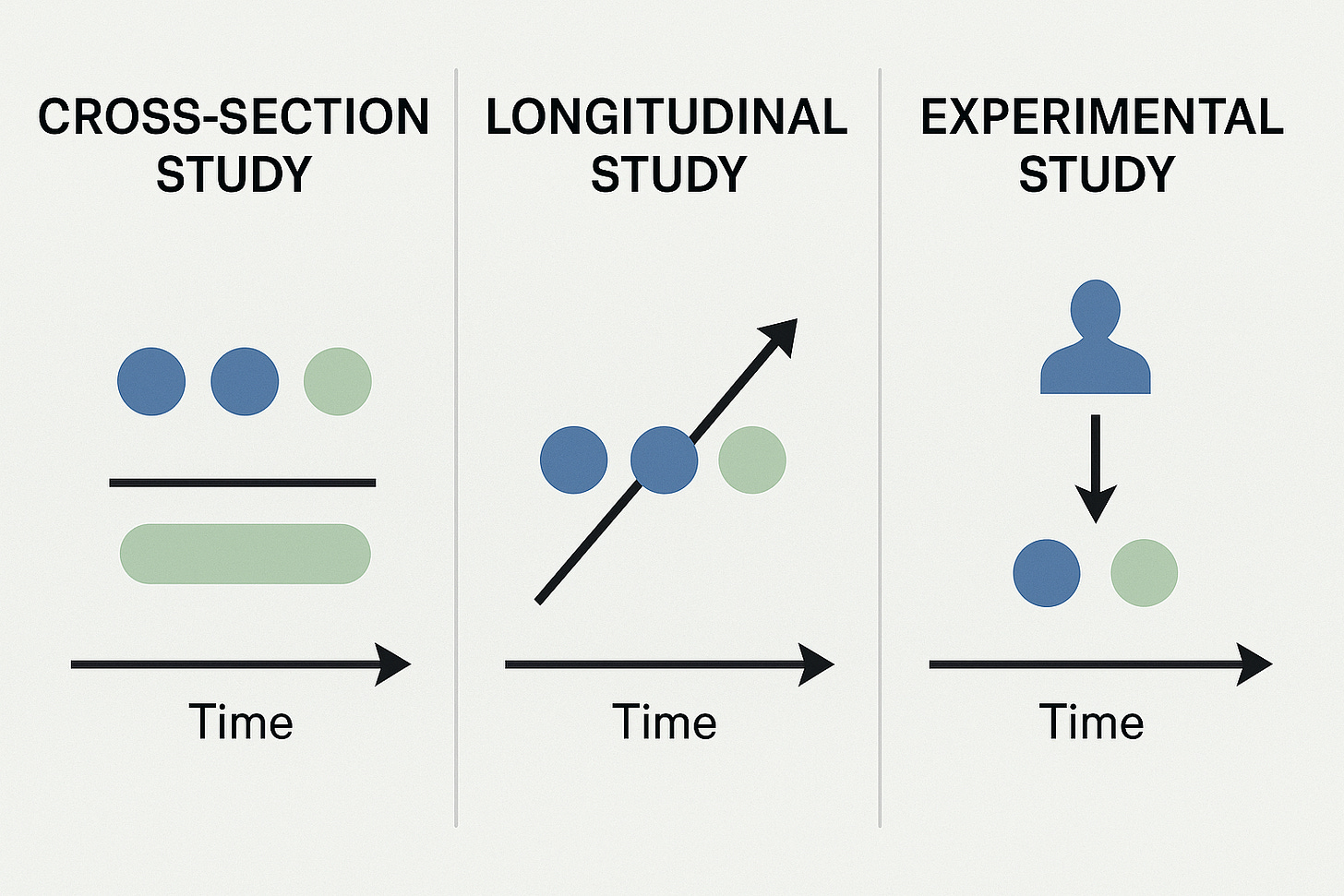
At its core, this was an epidemiological review—not a clinical trial. That means it can identify patterns, but not prove what caused them.
The findings? A modest increase in cardiovascular events—like acute coronary syndromes (ACS) and stroke—among cannabis users. Relative risks ranged from 1.03 to 1.36 depending on the study. And sure, those numbers are technically “statistically significant.” But here’s the catch:
With more than 400 million records, even tiny effects can pass the significance test. Think of it this way: if you surveyed every single person at Coachella about how many sneezes they had last week, something would look significant. But would it mean anything?
Or as one sharp reviewer once said:
“Statistical power without precision is just noise in disguise.”
(💭 What do YOU think—should studies with weak signal strength be treated as scientific leads, or media bait? Drop your thoughts in the comments.)
🧩 Part 2: Confounders, Confounders, Confounders
One of the study’s most glaring weaknesses isn’t buried in the fine print—it’s central to the entire premise: they couldn’t control for why people were using cannabis in the first place.
Many people turn to cannabis for chronic pain, PTSD, anxiety, or sleep disorders—all of which are themselves associated with increased cardiovascular risk. If someone’s heart is already under strain from chronic stress or years of poor sleep, cannabis use might be a bystander, not a culprit.
And guess what? Most of the studies included didn’t adequately adjust for those variables. That leaves us with an old research pitfall: confusing correlation with causation.
It’s like blaming coffee for everyone being tired—without asking why they needed it to begin with.
📣 Do you think researchers should have to clearly separate intent of use before publishing conclusions like these? Or is that too tall an ask for population studies? Chime in below.
📚 Quick Break: For Readers Who Want the Full Picture
If you’ve ever wished cannabis care came with a smarter instruction manual—good news. I wrote one:
👉 The Doctor-Approved Cannabis Handbook is the guide I wish every patient (and provider) had before stepping foot into a dispensary.
It’s science-forward, stigma-free, and full of the kind of real-world insights that don’t usually make it into clinical trials or cable news. If you’re tired of Googling and guessing—this one’s for you.
(Yes, I’m biased. But thousands of readers—and a few pleasantly surprised skeptics—agree.)
🔬 Part 3: Cannabis Isn’t One Thing—So Why Treat It Like It Is?
Another head-scratcher: this entire analysis lumps all cannabis use into one big basket.
Daily medical cannabis use for neuropathy? Toss it in. Weekend recreational edibles? Toss it in. One-time experimentation in high school? Toss it in. There’s no breakdown by formulation, frequency, route of administration, or even legal status.
And yet, conclusions are drawn as if we’re dealing with a single, uniform pharmaceutical compound.
Only one study in the entire review looked at medical cannabis directly (Zongo et al.), and even that relied on a proxy—prescription records—not actual patient usage, dosing, or product details.
No distinction between high-THC, CBD-dominant, or balanced formulations. Nothing about smoking versus capsules, tinctures, or topicals. That’s like doing a study on “food” and trying to link it to cholesterol without asking what people actually ate.
So when a meta-analysis doesn’t know if you used a gummy, a vape pen, or a suppository—how strong can its cardiovascular conclusions really be?
🎯 Have you noticed the way media headlines treat all cannabis the same—regardless of form or use? Hit share if that’s ever bugged you too.
One referral = one month free. That’s 100% off, mathletes:
🧭 Part 4: Public Health Trends Say Otherwise
Here’s the thing: if cannabis really were driving a meaningful uptick in cardiovascular events, we’d likely see that play out in real-world data. But instead, the epidemiologic landscape is... weirdly quiet.
In states where cannabis has been legal (and widely used) for years, we haven’t seen a spike in heart attacks, strokes, or ER admissions for cardiac events. No wave of cannabis-induced myocarditis. No surge of stroke among thirty-somethings grabbing edibles.
In fact, some public health trends move in the opposite direction. Cannabis users often report lower body mass index, reduced alcohol intake, improved insulin sensitivity, and in some cases, better sleep—all factors that arguably protect cardiovascular health.
And still, this meta-analysis gives those patterns little airtime. It’s like focusing on the potholes in a road and ignoring the entire four-lane highway built next to them.
⚖️ Are we missing the forest for the trees when we ignore public health context in favor of cherry-picked associations? Would love your thoughts below.
📎 Part 5: What This Paper Actually Tells Us
Let’s give credit where it’s due: this study was ambitious. Pooling this much data is no small feat. And yes, we absolutely should be scrutinizing the long-term cardiovascular effects of all widely used substances—including cannabis.
But let’s also be real. This paper is not a call for panic. It’s a call for better research.
We need cleaner definitions of exposure, stronger control for confounders, and—frankly—some humility about what these kinds of studies can and can’t tell us.
At best, this paper raises a hand and says, “Hey, let’s look deeper.” At worst, it risks fueling public misunderstanding with premature, poorly contextualized claims.
And for those who want the full technical unpacking—including a breakdown of each major limitation—check out the full write-up here:
🔗 https://www.cedclinic.com/cannabis-cardiovascular-risk
😄 Just for Laughs:
Why did the cannabis researcher fail at cooking?
Because they couldn’t control for thyme.
(Did you know CED Clinic has a free, full online cannabis cookbook?)
🗳️ Poll #1:
🗳️ Poll #2:
🧭 Want to Explore More?
For those of you who enjoy digging beneath the headlines—or debating them over dinner—here’s where to go next:
🔬 Full Technical Breakdown with Clinical Commentary
📍 A Much Deeper In-Depth Analysis on CEDclinic.com
📄 The Full Meta-Analysis Itself
📍 Read the Original Study (PDF)
🗞️ Recent Media Coverage Worth Scrutinizing
📍 New York Times: “Marijuana’s Links to Heart Attack and Stroke”
📍 CNN: “Marijuana Use Linked to Heart Disease and Death”
If you’ve made it this far, clearly you’re my kind of reader—curious, skeptical, and allergic to oversimplified headlines.
🗨️ What’s your take? Are we overstating risk—or finally facing uncomfortable truths? Join the conversation by sharing, commenting, or helping me promote a more balanced view.
📨 Found this helpful? Frustrating? Funny?
If you enjoy this content, help me sustain it Subscribe, share, and comment.
More: Here’s a 30-minute talk I gave recently. My version of a Cannabis 101: