Expecting & Experimenting
Why Cannabis in Pregnancy is More Mystery Than Medicine
Talking about cannabis and pregnancy can feel overwhelming, with strong opinions and mixed messages coming from all directions. This post cuts through the noise with an honest, evidence-based look at what we actually know. It’s not here to push an agenda—no glorification, no scare tactics—just a clear, thorough discussion of the science, the concerns, and the real questions people are asking.
You’ll find perspectives from both medical professionals and patients, along with research-backed insights to help make sense of a complex topic. The goal isn’t to tell you what to think, but to give you the best information available so you can engage in informed conversations—whether with your doctor, your patients, or your loved ones.
If something here sparks a question or a thought, jump into the comments. Share your experiences. Let’s have a real discussion. And if you know someone who could benefit from this, feel free to pass it along—because knowledge is most powerful when we share it.
Table of Contents
1. The State of Knowledge on Cannabis & Pregnancy
a. Background: The Rising Use of Cannabis During Pregnancy
b. Why More Pregnant Individuals Are Turning to Cannabis
c. What Do We Actually Know?
2. Research Challenges in Cannabis & Pregnancy
a. Lack of Randomized Controlled Trials (RCTs)
b. Confounding Variables
c. Differentiating Between THC and CBD
d. Correlational Versus Causal Outcomes
e. Product Variation and Standardization Issues
f. Other Key Scientific Gaps
3. Key Concerns: What Science Is Trying to Understand
a. Fetal Development
b. Placental Function & Pregnancy Outcomes
c. Maternal Health & Risk-Benefit Considerations d. A Tale of Two Studies and the Shifting Science
4. How Cannabinoids Interact with Pregnancy
a. The Endocannabinoid System (ECS) in Pregnancy
b. THC vs. CBD: A Side-by-Side Comparison
c. Timing Matters: Early vs. Late Pregnancy Effects
i. First Trimester – The Foundation Stage
ii. Second & Third Trimester – Growth and Maturation
d. Does Dose & Frequency Matter?
e. Consumption Methods & Their Implications
f. Polysubstance Use: Is Cannabis the Main Factor?
5. Weighing Risks and Benefits: Decision-Making in a Data-Poor Environment
a. Potential Risks of Cannabis Use During Pregnancy
b. Potential Benefits in Specific Clinical Scenarios
c. Challenges with Existing Therapies and Why Some Turn to Cannabis
d. Final Thoughts on Risk-Benefit Balancing
6. Cannabis & Pregnancy Frequently Asked Questions (FAQ)
7. Historical Timeline and Key Research Findings
8. Summary and Recommendations
9. Future Directions and Research Priorities
10. Case Studies and Vignettes
A sample case study, more in text below!
11. Glossary of Terms
12. Comprehensive Evidence (References with PDFs) & Sources
13. The Executive Summary (tl;dr)
14. Resources to Learn More
1. The State of Knowledge on Cannabis & Pregnancy 🌐
This document provides an in‐depth, evidence‐driven exploration of the current knowledge, debates, and clinical realities regarding cannabis use during pregnancy, in 2025. It is intended to be a reference for both patients and providers, balancing scientific nuance with practical insights. The full PDFs for all reference materials are linked and free to read.
a. Background: The Rising Use of Cannabis During Pregnancy
Over the past decade, cannabis use among pregnant individuals has surged. Broader legalization, a prevailing perception of cannabis as a “natural” alternative, and dissatisfaction with conventional treatment options have all contributed to this trend. For example, one study found that self‐reported cannabis use increased from 3.4% in 2002 to 7.0% in 2017—with the highest use in the first trimester (Corsi et al., 2019). It is important to note that underreporting likely means these numbers underestimate true consumption.
b. Why More Pregnant Individuals Are Turning to Cannabis
Pregnant individuals often turn to cannabis when conventional therapies fail to deliver relief or when traditional treatments come with intolerable side effects. Here are several common instances and additional examples that highlight the range of reasons behind this trend:
1. Severe Nausea and Hyperemesis Gravidarum (HG):
Many expectant mothers suffer from extreme morning sickness. In its most severe form—hyperemesis gravidarum—persistent nausea and vomiting can lead to dehydration, weight loss, and hospitalization. When standard anti-nausea medications are either ineffective or cause unwanted side effects, some turn to cannabis in search of relief.
2. Chronic Pain Conditions:
Conditions such as fibromyalgia, multiple sclerosis, or persistent back pain do not simply vanish during pregnancy. Standard pain relievers like NSAIDs and opioids are often contraindicated due to potential risks to the fetus. For these individuals, cannabis offers an alternative that many find effective for managing pain without the associated dangers of more conventional medications.
3. Mental Health Challenges:
Pregnancy can amplify existing mental health issues or bring on new challenges such as anxiety, depression, post-traumatic stress disorder (PTSD), and sleep disorders. Many pregnant individuals worry about the risks associated with traditional psychiatric medications, which might lead to neonatal withdrawal or other adverse effects. Cannabis, particularly non-intoxicating compounds like CBD, is sometimes used to alleviate these symptoms and promote a sense of calm.
4. Appetite Stimulation and Weight Management:
For some women, persistent nausea or other pregnancy-related changes can diminish appetite, leading to nutritional deficits that affect both mother and baby. Cannabis is known for its appetite-stimulating properties (“the munchies”), and in certain cases, it may help ensure that the expectant mother maintains an adequate nutritional intake.
5. Alleviation of Migraine and Headache Symptoms:
Migraines and severe headaches can be especially debilitating during pregnancy. Conventional treatments for migraines may be limited or pose risks during gestation, prompting some patients to explore cannabis as an alternative for managing headache-related pain and discomfort.
6. A Perception of Cannabis as a “Natural” Remedy:
With the wave of legalization and growing cultural acceptance, cannabis is often marketed as a natural, holistic alternative to pharmaceutical drugs. Dispensaries and online communities frequently share anecdotal success stories, leading many pregnant individuals to view cannabis as a safer, more natural option—especially when compared to the chemical composition of many traditional medications.
7. Influence from Peer Experiences and Online Communities:
Social networks, support groups, and online forums can play a significant role in shaping perceptions. Many pregnant individuals report hearing firsthand accounts from friends or community members about the positive effects of cannabis on symptoms such as nausea or chronic pain, thereby influencing their decision to try it themselves.
8. Unmet Medical Needs and Provider Gaps:
Sometimes, standard medical care does not adequately address the full spectrum of symptoms experienced during pregnancy. In cases where healthcare providers are not well-versed in alternative therapies, patients may turn to cannabis as a last resort after conventional options have been exhausted.
Think This Through: Which of these challenges do you or someone you know experience? Reflect on the specific symptoms that disrupt your daily life—whether it’s severe nausea, persistent pain, or overwhelming anxiety. How might the idea of using a more “natural” remedy influence your decision when traditional treatments aren’t providing enough relief?
Mental Health & Cannabis: Learn More
c. What Do We Actually Know?
Despite its growing popularity, the scientific evidence on cannabis use during pregnancy remains inconclusive. Unlike alcohol and tobacco—which have decades of longitudinal data—most cannabis research is observational. This forces clinicians and patients to sift through widespread rumors and lingering stigma while grappling with profound uncertainties about its true benefits and potential harms.
2. Research Challenges in Cannabis & Pregnancy 🔬
Research in this area faces many challenges, including difficulties in designing studies, ethical problems, and everyday practical issues.
a. Lack of Randomized Controlled Trials (RCTs)
Randomized controlled trials are the best way to prove cause and effect, but it isn’t ethical to intentionally give cannabis to pregnant people without knowing it’s completely safe. As a result, most studies rely on observational data—using self-reports, medical records, or past data—which can lead to errors like incomplete recall or inaccurate estimates of cannabis use. In addition, many research subjects take other medications, face high levels of stress, have varied recreational habits, sleep patterns, and nutritional baselines. All these factors make it challenging to pinpoint the exact impact that cannabis might have on both mother and baby.
Think This Through: Imagine you’re using cannabis during pregnancy and you’ve read that, because studies haven’t been able to control for all the other factors—like smoking, diet, and stress—we can’t be 100% sure that cannabis alone causes certain issues. How does that uncertainty affect your own feelings about using cannabis? Do you feel more cautious because you wish you had clear answers, or do you think that other aspects of your lifestyle might be playing a bigger role?
b. Confounding Variables
Many studies have a hard time showing that cannabis alone is responsible for the effects seen during pregnancy. This is because many pregnant people who use cannabis also smoke tobacco, drink alcohol, or face significant challenges such as poverty or food insecurity. These other factors are well known to cause serious issues—like babies being born too early or with low birth weight—and this has been demonstrated repeatedly in robust, reproducible research over many years. Because these influences are so well established, it becomes very difficult for researchers to determine exactly how much of the risk is due to cannabis itself versus these other factors.
For example: imagine a scenario where a pregnant woman regularly uses cannabis to help manage nausea, but she also smokes cigarettes daily and struggles with food insecurity. When her baby is born prematurely and with a low birth weight, it’s difficult for researchers to determine which factor—cannabis, tobacco, or poor nutrition—played the primary role. We know from robust, long-term studies that tobacco use and inadequate nutrition are strong, well-documented causes of these outcomes. But, because these factors often come together, it becomes difficult to separate out the specific impact of the cannabis. This is why scientists rely on carefully designed studies that try to account for all these overlapping influences, but even then, pinpointing the exact contribution of cannabis is incredibly complex.
Think This Through: Imagine you’re a pregnant woman who has struggled with a strong cigarette habit and finds it too hard to quit completely. So, you manage to cut down on smoking, but you also use cannabis to help ease the anxiety and cravings. Now, if your baby is born prematurely or with a low birth weight, take a moment to reflect: do you believe these outcomes might be more related to the residual effects of smoking, the use of cannabis, or a combination of both? How do you feel each habit might be affecting your pregnancy, and what steps could you consider to improve your overall health and that of your baby?
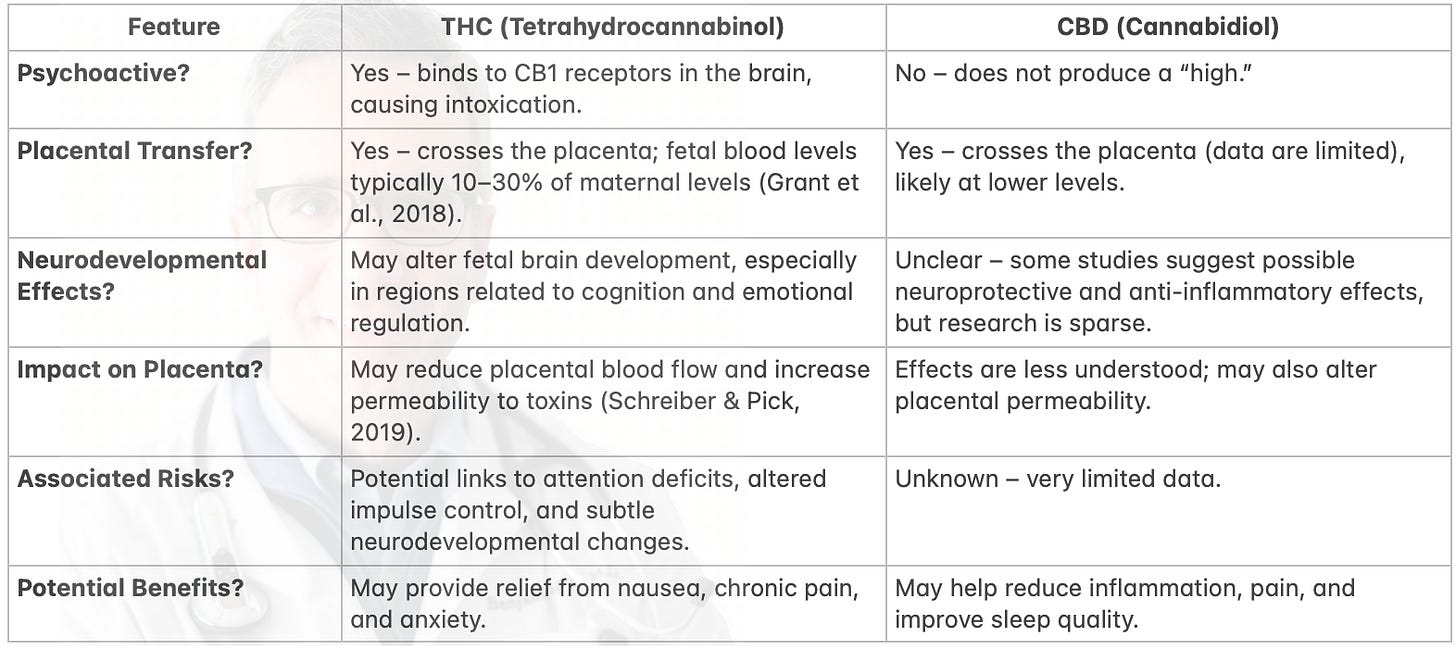
c. Differentiating Between THC and CBD
One major limitation of current research is that many studies fail to distinguish between the two main cannabinoids: THC and CBD. THC produces euphoria by binding to CB1 receptors in the brain and mimics anandamide—a naturally occurring chemical found in everyone—which, like THC, crosses the placenta during pregnancy. In contrast, CBD is non-intoxicating and is known for its pain-relieving, anti-inflammatory, and neuroprotective properties. Furthermore, THC and CBD can affect various organs differently—sometimes even having opposite effects, such as stimulating versus inhibiting tissue growth. When studies don’t differentiate these compounds, it becomes nearly impossible to determine whether the observed outcomes are due to THC alone, CBD alone, or a combination of both.
Think This Through: Imagine trying to perfect your favorite recipe but not knowing which spice is responsible for an unexpected flavor. Without that knowledge, you wouldn’t know what to adjust, and your final dish might turn out unpredictable. Now, picture a pregnant woman who worries that using cannabis might harm her baby’s brain development—even though the specific cannabis products she uses may not actually bind directly to her baby’s brain receptors. Consider further that a mother’s overall mood, reflected by her natural endocannabinoid tone, plays a significant role in her baby’s growth. For example, a depressed mother may have a low natural endocannabinoid tone, while a cheerful, vibrant mother might naturally have a higher tone. If these differences exist naturally, should we view a mother’s decision to use external cannabinoids (to boost her tone) any differently than if she had chosen to eat extra healthy foods during pregnancy? Reflect on how these factors—just like the missing spice in your recipe—can complicate the picture of maternal health and decision-making.
d. Correlational Versus Causal Outcomes
Most research in this area is correlational. Studies may find associations between prenatal cannabis exposure and outcomes such as low birth weight or neurodevelopmental delays, but they cannot prove that cannabis is the direct cause of these effects. Imagine how, in everyday life, we often see two events happen together and jump to the conclusion that one must cause the other—for example, noticing that ice cream sales and drowning incidents both rise during the summer and assuming one causes the other. This kind of thinking is natural; our brains are wired to infer causation from correlation because it simplifies complex information.
Now, consider a pregnant woman who uses cannabis and also experiences high stress, or perhaps she lives in an area with significant environmental pollution. If her baby is born with a low birth weight, it can be very confusing: is the outcome due to cannabis use, the stress she’s under, or the exposure to toxins in her environment? Researchers know that factors like maternal stress, exposure to environmental toxins, and concurrent use of substances such as tobacco or alcohol are well-documented causes of adverse outcomes like low birth weight and premature birth. These factors have been repeatedly confirmed by robust, reproducible studies over time.
Because so many variables can be at play, the simple correlation between cannabis use and a particular outcome may not reflect a direct cause-and-effect relationship. Instead, these overlapping influences can lead to misinterpretations. The social human brain is naturally inclined to make quick, causal inferences from correlated events, even when such connections might be misleading. This confusion—prevalent among both the general public and, at times, even within the scientific community—underscores the need for careful, controlled studies to tease apart the precise impact of cannabis from the effects of other co-occurring risk factors.
Think This Through: Imagine you’re trying to figure out if your daily cup of coffee is causing your headaches. To be sure, you’d need to compare days when you have coffee with days when you don’t—under similar conditions—and see if the headaches reliably appear only when you drink coffee. Similarly, to confidently say that cannabis exposure is directly causing adverse outcomes in pregnancy, researchers would need evidence that isolates cannabis as the sole variable. This would involve controlled studies that account for other factors—like tobacco use, stress, and nutrition—and demonstrate a consistent dose-response relationship where increasing cannabis exposure leads to predictable increases in risk. How do you think such clear, controlled evidence would change your perspective on the potential risks?
e. Inconsistent Cannabis Formulations and the Need for Uniformity
Cannabis is not a standardized pharmaceutical product—its composition can vary widely based on strain, cultivation method, and the type of product used (flower, concentrates, edibles, or vapes). For example, early research typically examined cannabis with only 2–5% THC, whereas many modern products contain 15–30% THC or more. Imagine if everything we knew about bananas came only from studying rotten ones—the conclusions would be skewed. Likewise, findings from older or inconsistent cannabis products may not accurately represent the characteristics of today’s formulations. Moreover, even if modern products are grown and sold to be more potent, we also don’t know if people are consuming them in the same amounts or with the same frequency as before. This variation in both product composition and consumption patterns further complicates efforts to compare past research with current real-world use.
Think This Through: Imagine two pregnant women who use cannabis. One chooses a product with a lower THC level and uses it occasionally, while the other opts for a highly potent product and uses it daily. The differences in dosage and frequency could lead to very different outcomes for their babies. How might these contrasting scenarios affect your understanding of the risks and benefits of cannabis during pregnancy?
f. Other Notable Scientific Gaps
Limited Research on Diversity: Many studies haven’t included people from different ethnic and financial backgrounds, so we don’t know if cannabis affects all groups of pregnant women in the same way.
Uncertainty About Post-Birth Health: We lack enough information on how using cannabis during pregnancy might impact a mother’s health after giving birth, including breastfeeding and recovery.
Not Enough on Drug Interactions: There’s little research on how cannabis interacts with other medicines taken during pregnancy, making it hard to understand the overall risks.
No Reliable Exposure Tests: Scientists still don’t have consistent tests to accurately measure how much cannabis a pregnant woman or her baby is exposed to, which makes it difficult to know the exact dose.
How It Works at a Cellular Level: We need more studies to clearly explain how the chemicals in cannabis affect cells and organs during pregnancy.
Little Data on Other Cannabis Chemicals: While we know a lot about THC and CBD, there’s very little information on the other chemicals in cannabis and how they might affect health.
Missing the Bigger Picture: Many studies don’t fully consider other factors like pollution, stress, or lifestyle habits, which could work together with cannabis use to affect pregnancy outcomes.
Effects Before Pregnancy: We haven’t looked closely at how using cannabis before pregnancy might have lingering effects on a baby’s development.
Multiple Exposures Confuse the Issue: When cannabis is used along with other substances like tobacco or alcohol, it becomes hard to tell which one is causing a particular problem.
Limited Long-Term Follow-Up: Most research only follows babies for a short time after birth, so we have little information on how prenatal cannabis exposure might affect children as they grow, especially when combined with other environmental factors.
Genetic Differences in Cannabis Metabolism: People have different genes that affect how quickly their bodies break down cannabis. For example, variations in enzymes like CYP2C9 and CYP3A4 can mean one woman might have cannabis in her system longer than another, even if they use the same amount.
Lack of Detailed Dose-Response Data: There isn’t enough information to compare occasional, low-dose use with daily, high-dose consumption, making it hard to know what levels might be safe or risky during pregnancy.
Think This Through: If you could choose one research gap to focus on—whether it’s understanding how genetic differences affect cannabis metabolism, obtaining precise dose-response data, or tracking children’s development into later years—which would you prioritize? Consider how closing that gap might change our understanding of how prenatal cannabis exposure impacts both mothers and their babies. Now you can start to understand some of the challenges that scientists face in disentangling these complex factors.
3. Key Concerns: What Science Is Trying to Understand 🤔
Researchers have found a few important issues that still need more study so that doctors can make better decisions.
a. Fetal Development
Fetal development is extremely delicate, especially during the time when the baby’s organs and brain are just starting to form. Research shows that THC—the main active ingredient in cannabis—can pass from the mother to the baby, with the baby ending up with about 10–30% of the THC that the mother has in her blood (Grant et al., 2018). This matters because the baby’s brain relies on a natural system, called the endocannabinoid system (ECS), to build the connections between brain cells. When THC gets into this system, it might interfere with how these connections are made. Studies in animals suggest that such interference could change the way dopamine, a compound that is important for focus and reward, is managed, which might lead to issues with attention or behavior later in life.
An example that illustrates well the swings in cannabis literature, that may help explain the swings in cultural understanding comes between ,
b. Placental Function & Pregnancy Outcomes
The placenta acts as the baby’s lifeline, supplying essential nutrients and oxygen from the mother. Some studies suggest that cannabis use during pregnancy might reduce the placenta’s blood flow and make its barrier more permeable, or “leaky.” This disruption in placental function can lead to complications such as the baby not growing as expected, increased risk of high blood pressure during pregnancy, and even preeclampsia—a serious condition marked by sudden, severe high blood pressure that can damage the mother’s organs and endanger both mother and baby.
While large studies have linked cannabis use to outcomes like low birth weight and early delivery, it’s important to note that these associations are often complicated by other factors, such as tobacco use, stress, or poor nutrition. This means that although cannabis may contribute to these issues, it is difficult to isolate its impact from other influences that also affect pregnancy outcomes.
In many cases, cannabis is considered a last resort when traditional treatments fail to provide relief. For example, a pregnant woman suffering from severe hyperemesis gravidarum may experience intense, persistent nausea and vomiting that lead to dehydration, significant weight loss, and even hospitalization. Similarly, individuals with chronic pain conditions—such as fibromyalgia or persistent back pain—might find that conventional pain relievers are either unsafe or ineffective during pregnancy. Mental health challenges like anxiety and depression can also worsen during pregnancy, especially when standard medications bring unwanted side effects or pose potential risks.
In these challenging situations, the decision to use cannabis involves weighing the immediate dangers of untreated symptoms against the uncertain long-term effects on the baby. Research has shown that severe maternal stress, dehydration, and malnutrition can negatively impact fetal growth and development. Many patients report significant symptom relief with cannabis, but its long-term impact on the fetus remains unclear. This creates a difficult balancing act: the known harms of leaving severe symptoms untreated may be substantial, yet the effects of cannabis exposure are still not fully understood.
Moreover, each woman’s situation is unique. Individual differences in biology, the severity of symptoms, and overall health make it essential for healthcare providers to tailor their advice to each patient. Clinical experience often shows that real-world outcomes are more complex than what studies alone can capture. In some cases, when traditional therapies are inadequate, a carefully managed cannabis regimen might offer a lower overall risk compared to the known dangers of untreated conditions. However, because long-term outcomes are still uncertain, decisions must be made on a case-by-case basis through open, honest discussions between patients and their healthcare providers.
Women’s Health & Hormones: Learn More
Think This Through: Imagine you’re a pregnant woman suffering from severe, debilitating symptoms—constant nausea that makes eating nearly impossible or chronic pain that disrupts your daily life. These symptoms not only lower your quality of life but can also harm your baby by creating a stressful environment and limiting the nutrients it receives. Now, picture yourself discussing these challenges with your healthcare provider. You both weigh the well-documented risks of untreated symptoms—such as dehydration, weight loss, and stress—against the uncertain long-term effects of a carefully managed cannabis regimen. At the same time, consider the provider’s perspective: when standard treatments fail, is it ethical to recommend a treatment that might offer relief even though its impact on fetal development isn’t fully understood? Both of you might ask, “Could my persistent pain or severe nausea be more dangerous than the potential, yet not clearly defined, risks of using cannabis?” You would explore options like using lower doses or alternative consumption methods to minimize exposure. This shared, open conversation—balancing the immediate need for relief with the duty to protect your baby—illustrates the complex challenges both patients and providers face when making informed decisions in the face of uncertainty.
d. A Tale of Two Studies and the Shifting Science
An example that perfectly captures the swings in cannabis research—and the resulting shifts in public perception—comes from two studies led by many of the same authors. One, published in The American Journal of Obstetrics & Gynecology, found that babies exposed to cannabis in utero had a higher likelihood of being born underweight, arriving preterm, or needing NICU care . The conclusion? Cannabis exposure during pregnancy might pose significant risks to newborns.
But then, in another study published in JAMA Network Open, the same research team looked at a different angle—child development over time. Tracking kids up to age 5.5, they found no link between prenatal cannabis exposure and early developmental delays, including speech, motor skills, or overall cognitive development .
So, what does this tell us? On one hand, cannabis exposure during pregnancy may affect immediate birth outcomes. On the other, those early disadvantages don’t necessarily translate into measurable developmental struggles down the line. It’s a striking contrast—one study warns of possible harm at birth, while the other suggests those harms may not persist as the child grows.
This kind of whiplash in the literature fuels the broader cultural uncertainty around cannabis and pregnancy. The reality is, science evolves. What seems like a clear risk today can look more nuanced when examined through a wider lens. That’s why ongoing research—and an open, critical approach to new data—is so important in shaping how we think about cannabis and health.
4. How Cannabinoids Interact with Pregnancy 🧬
Understanding how cannabinoids affect a pregnant body is essential for weighing their potential benefits against any risks. The body’s natural endocannabinoid system (ECS)—a complex network that regulates processes like fetal brain development, placental function, and overall maternal health—plays a central role during pregnancy. Despite decades of research since its discovery in 1992, there is still much we do not fully understand about how the ECS influences pregnancy. Yet, significant effort, concern, and debate continue as scientists work to unravel the effects of plant-based cannabinoids on these natural systems. When external cannabinoids from cannabis interact with the ECS, they can alter these critical processes in various ways, sometimes leading to unexpected outcomes. This section explores these interactions, the underlying science, and what they might mean for pregnant individuals considering cannabis use.
a. The Endocannabinoid System (ECS) in Pregnancy
The endocannabinoid system (ECS) is like your body’s internal balancing act—it helps regulate everything from immune function and brain development to appetite, stress response, and even sleep. The ECS is made up of naturally produced chemicals called endocannabinoids, such as anandamide and 2-AG, along with receptors that detect and respond to these chemicals. You might have heard of the well-known CB1 and CB2 receptors, but the ECS also involves many other important receptors like TRPV1, GPR55, GPR18, PPARα, and PPARγ. These additional receptors help fine-tune processes ranging from pain perception and inflammation to metabolism and cell growth. In everyday life, the ECS influences how you experience pain, regulate your hunger (think of the “munchies”), manage stress, and even affect your mood and memory.
During pregnancy, the endocannabinoid system (ECS) plays a critical role. It helps the embryo attach to the uterus by maintaining proper levels of natural chemicals like anandamide, which create an ideal environment for implantation. The ECS also supports placental development by guiding cell growth and encouraging the formation of healthy blood vessels, ensuring that the fetus receives sufficient nutrients and oxygen. Moreover, the ECS influences the developing brain by affecting how nerve cells connect—a process that is essential for future learning and behavior. For example, balanced anandamide levels are key for successful implantation, and disruptions in this balance may contribute to early pregnancy loss (Costa, 2016). This delicate equilibrium highlights the importance of the ECS not only for everyday bodily functions but also for laying the foundation of a healthy start to life.
b. THC vs. CBD: A Side-by-Side Comparison
Here, a table comparing the two most popular cannabinoids, summarizing their known effects and highlighting areas where data are limited:
Think This Through: Consider that in the U.S. today, CBD is fully legal while THC remains federally illegal, even though many states allow it in some form. Yet, despite these legal distinctions, neither federal nor state agencies are formally tracking the safety and effectiveness of these products. What might this lack of formal monitoring suggest about the perceived risks of cannabis? More importantly, does it prompt a question about whether the government should be influencing health decisions related to cannabis, or should these choices rely more on independent research and individual judgment? Reflect on whether it makes sense for government policy to guide personal health decisions when systematic safety tracking is not in place.
c. Timing Matters: Early vs. Late Pregnancy Effects
The impact of cannabis during pregnancy can differ dramatically depending on when exposure occurs. In the earliest weeks—when the baby’s organs and basic structures are just beginning to form—even small amounts of cannabis may disrupt critical developmental processes. Later in pregnancy, as the baby’s brain matures and more complex neural connections are established, cannabis exposure might influence subtler aspects of brain function, potentially affecting learning, behavior, or other cognitive skills. Understanding these timing differences requires looking closely at the key milestones in fetal growth and considering the ongoing debates among experts regarding the true implications of cannabis exposure at various stages. This nuanced perspective is essential for making informed decisions about the risks and benefits associated with cannabis use during pregnancy.
First Trimester – The Foundation Stage
During the first trimester (0–12 weeks), the embryo develops at an astonishing rate. This is when the basic blueprint of the baby is established. Key events include:
Neural Tube Formation: The neural tube, which later develops into the brain and spinal cord, begins to form.
Early Brain Development: The initial structures of the brain start to emerge.
Heart Function: The heart starts beating around week 6.
Organogenesis: Vital organs like the kidneys, liver, and pancreas begin to develop.
Theoretical Concerns:
Some experts worry that external cannabinoids, particularly THC, might interfere with these critical developmental processes. The body’s natural endocannabinoid system (ECS), discovered in 1992, helps guide how nerve cells connect and tissues form. Laboratory and animal studies have shown that when THC binds to receptors such as CB1, it can alter the normal migration of nerve cells or the formation of synapses. This disruption could theoretically lead to subtle cognitive or behavioral issues later in life.
Clinical Evidence:
Real-world studies, however, do not consistently show a clear pattern of birth defects or major physical problems directly linked to cannabis use during the first trimester. Epidemiological research has not identified a specific “cannabis teratology syndrome,” suggesting that while there may be risks, they are not as clear-cut as some laboratory findings might imply.
Alternate Perspective:
Interestingly, some researchers propose that for mothers with naturally low levels of endocannabinoids—a condition only recognized since the ECS was discovered—a carefully managed use of external cannabinoids might help restore balance, much like taking vitamins to correct a deficiency. Although this theory is still speculative, it highlights that the effects of cannabis on early development are complex and may vary significantly from one individual to another.
Second & Third Trimester – Growth and Maturation
During the later stages of pregnancy (from about 13 to 40 weeks), the baby experiences rapid growth and significant maturation. Not only does the fetus increase in size and weight, but crucial systems are refined:
Brain Development: The brain grows rapidly, forming a complex network of nerve connections. The process of myelination—where nerve fibers are coated to improve signal transmission—is well underway, laying the foundation for future learning and behavior.
Organ Maturation: Organs such as the lungs, liver, and kidneys continue to mature, preparing the baby for life outside the womb.
Placental Function: The placenta continues to play its vital role by ensuring that the baby receives the nutrients and oxygen it needs while removing waste products.
Theoretical Concerns:
Some experts worry that ongoing cannabis exposure during the second and third trimesters could subtly disrupt these finely tuned processes. For example, THC might alter the way the brain’s chemical messengers work or interfere with the signals that help maintain healthy blood flow through the placenta. Such interference could, in theory, contribute to complications like lower birth weight or even premature birth if the placenta cannot supply enough nutrients and oxygen.
Clinical Evidence:
In real-world studies, however, there is no definitive link between prenatal cannabis exposure during these later stages and major developmental defects. While some research has noted small associations with outcomes such as low birth weight, these findings are often muddled by other factors like tobacco use, high stress levels, or poor nutrition—making it hard to pinpoint cannabis as the sole cause.
Alternate Perspective:
Some researchers also propose that if a mother’s natural endocannabinoid levels are suboptimal, additional cannabinoids might actually help support normal growth and maturation during these critical stages. Just as vitamins can correct a nutritional deficiency, cannabinoid supplementation could, in theory, help restore balance. However, this idea remains under investigation and is not yet confirmed.
These considerations illustrate how the timing of cannabis exposure during pregnancy can have different potential effects, and why the issue is so complex. In both early and later stages of pregnancy, the interactions between cannabis, the endocannabinoid system, and various developmental processes require further study. Understanding these nuances is essential for making informed decisions about cannabis use during pregnancy.
Think This Through: Consider how cannabis exposure during the early stages of pregnancy—when the embryo’s basic structures and organs are just forming—might have very different effects compared to exposure later, during the period of rapid growth and maturation. Early exposure could potentially disrupt critical developmental processes, while later exposure might have a less pronounced effect. How does one weigh these theoretical risks against clinical evidence that doesn’t clearly show significant harm?
Now, consider the opposite perspective: if a mother’s natural endocannabinoid system is underactive or deficient, her baby might suffer from a lack of essential signals needed for proper development. For example, imagine a situation similar to a child with a vitamin deficiency; when the deficiency is corrected through supplementation, the child’s health improves significantly. In such cases, could using cannabinoids help restore a healthier balance and support the baby’s development? And if so, is it ethical to withhold cannabis when traditional treatments aren’t providing relief? Reflect on these contrasting views to appreciate the complexity of making informed health decisions during pregnancy.
d. Does Dose & Frequency Matter?
Cannabis use isn’t one-size-fits-all. The frequency of use, the amount consumed, and the method of consumption (such as smoking, vaping, or edibles) can lead to very different effects on the body. For example, a person who uses cannabis only occasionally may experience minimal impact, whereas someone who uses it daily in high doses could face much greater risks. In addition, differences in product strength and the way it’s delivered add further complexity. Unfortunately, many studies lump all these different patterns together, making it difficult for healthcare providers to offer truly personalized and precise advice.
Think This Through: Imagine trying to judge the safety of a medication without knowing its exact dose or how often it’s taken. How important is it to accurately measure both the amount and frequency of cannabis use when evaluating its potential risks during pregnancy? And when you consider the countless variables—differences in individual biology, diverse environmental factors, and the wide range of cannabis products and usage methods—at what point should care and guidance be completely tailored to each person rather than relying on one-size-fits-all recommendations?
e. Consumption Methods & Their Implications
For pregnant women, the way cannabis is consumed can affect both the mother’s body and the developing fetus in distinct ways. Different methods lead to varying levels of exposure to active compounds such as THC, which is particularly important when considering the potential impact on fetal development. Below is a breakdown of common consumption methods and their specific implications for pregnancy:
Smoking & Vaping
How It Works:
Cannabis is inhaled, allowing THC to rapidly enter the bloodstream through the lungs.
Effects on Pregnancy:
The fast absorption offers quick relief, which might be beneficial in acute situations. However, smoking produces harmful byproducts like carbon monoxide, which can reduce the oxygen supply to both the placenta and the fetus. Vaping may reduce some toxins but still delivers high peak levels of THC quickly, potentially increasing fetal exposure.
Realistic Impact Considerations:
While some studies have linked smoking cannabis during pregnancy to adverse outcomes such as low birth weight and preterm birth, these findings are often complicated by concurrent tobacco use and other lifestyle factors. The rapid delivery of THC is a theoretical concern, but real-world data have been mixed. Overall, the risks may be higher with smoking due to the added exposure to combustion byproducts, yet the precise degree of harm remains difficult to isolate.
Edibles
How It Works:
Cannabis is infused into food or beverages and then ingested, leading to absorption through the digestive system.
Effects on Pregnancy:
Edibles have a slower onset of effects and tend to produce a prolonged exposure to THC. The absorption rate can vary widely based on factors such as metabolism and the presence of other foods, which means the fetus might be exposed to THC over a longer period, even if the peak levels are lower.
Realistic Impact Considerations:
Although the prolonged exposure from edibles is concerning in theory, published data on the specific effects of edibles during pregnancy are limited. The variable absorption makes it hard to determine a consistent risk level. Some observational studies hint at developmental differences, but it is not yet clear whether these are directly attributable to the extended exposure pattern seen with edibles.
Tinctures
How It Works:
Cannabis tinctures are liquid extracts taken sublingually (under the tongue), which allows for faster absorption than edibles without the risks associated with inhalation.
Effects on Pregnancy:
Tinctures provide more controlled and predictable dosing, with a moderate onset of effects. This method avoids the harmful byproducts of combustion, making it a potentially safer option.
Realistic Impact Considerations:
Although tinctures offer a more precise dosing method, there is limited research specifically examining their impact during pregnancy. Theoretically, if the dosage is well controlled, the risks to the fetus may be lower compared to smoking or vaping. However, without robust studies, it is difficult to say with certainty how tinctures compare in terms of fetal safety.
Topicals
How It Works:
Cannabis-infused creams, balms, or lotions are applied directly to the skin for localized relief.
Effects on Pregnancy:
Topicals are designed to target specific areas for relief from pain or inflammation and typically do not result in significant systemic absorption of cannabinoids. This means they are unlikely to produce the psychoactive effects associated with THC.
Realistic Impact Considerations:
Because topicals do not generally enter the bloodstream in significant amounts, the risk of affecting fetal development is considered to be low. However, it is still important to consider product quality and potential contaminants. Overall, topicals are likely to be the safest form of cannabis use during pregnancy, provided they are used as intended and sourced from reputable manufacturers.
Each method of consumption produces different speeds and amounts of THC absorption. These differences can determine how much THC the fetus is exposed to, potentially influencing its development in unique ways. For pregnant women, understanding these nuances is crucial for making informed decisions about cannabis use, as even small variations in consumption patterns may have different implications for maternal and fetal health.
Think This Through: The way cannabis is consumed—whether by smoking, vaping, eating edibles, or using tinctures and topicals—can significantly affect both the immediate and long-term outcomes for the fetus. Different methods deliver cannabinoids at varying speeds and concentrations, which means the amount of THC that actually reaches the baby can differ greatly. This variability makes it hard for researchers to study the effects consistently because it’s challenging to ensure everyone uses cannabis in the same way. In addition, a mother’s natural levels of endocannabinoids, like anandamide, may influence how her body and her baby respond to these external compounds. Without taking these factors into account, it’s difficult to draw clear conclusions about the true risks and benefits of cannabis during pregnancy.
f. Polysubstance Use: Is Cannabis the Main Factor?
Many pregnant individuals who use cannabis also use other substances—such as tobacco, alcohol, or prescription medications. This pattern of combined use, known as polysubstance use, makes it difficult for researchers to pinpoint which substance is responsible for adverse outcomes. For instance, tobacco is well known for causing low birth weight and premature delivery, and alcohol is a confirmed teratogen that can lead to birth defects. When these substances are used together, it becomes challenging to isolate the specific effects of cannabis on pregnancy outcomes. This overlap highlights the need for studies that carefully control for these factors, as the cumulative impact of multiple exposures may be greater than the effect of any one substance alone.
Think This Through: When a pregnant woman uses more than one substance—such as cannabis along with tobacco or alcohol—it’s important for her and her doctor to consider all the factors at play. For example, since tobacco is known to cause low birth weight and premature birth, they need to ask: How much of these adverse outcomes might be due to smoking versus cannabis? They should also consider additional lifestyle factors like nutrition, stress, and overall health, which can further influence outcomes. Reflect on the importance of assessing each risk individually, so that both patient and provider can work together to understand which factors are most likely impacting maternal and fetal health.
5. Weighing Risks and Benefits: Decision-Making in a Data-Poor Environment ⚖️
When high-quality evidence is scarce, doctors must use a careful risk-benefit analysis tailored to each patient’s unique situation. In complex areas—like cannabis use during pregnancy—clinical judgment is as vital as academic research because studies often can’t capture the full picture of a patient’s health or the nuanced effects of treatment. For example, while a study might report average outcomes, a doctor in the clinic might observe subtle trends influenced by factors such as stress, nutrition, or lifestyle that haven’t yet made it into published research. These everyday observations are crucial for making informed decisions.
This reliance on real-world experience is especially pronounced in fields like surgery and palliative care. In surgery, while textbooks provide essential knowledge of anatomy and procedures, the true skill of a surgeon is built over years of hands-on practice—mastering technical techniques and making critical decisions in real time during operations. Similarly, palliative care doctors often deal with complex patient needs that involve not only medical treatments but also emotional, psychological, and social support. Much of what they learn comes from direct patient interactions and long-term relationships, rather than from textbooks alone.
In emergency medicine, clinicians must rapidly assess and treat patients under pressure, often relying on instincts developed through years of experience when textbook answers fall short. In primary care and psychiatry, doctors navigate intricate, individualized health issues where the “art” of medicine—gained through real-world practice and personal insight—is key to tailoring treatment effectively.
Just as an experienced chef adjusts a recipe based on the quality of ingredients and personal taste, clinicians use their firsthand experiences to fine-tune treatments when research doesn’t tell the whole story. This “crystal ball” perspective from the clinical office bridges the gap between controlled research and the unpredictable nature of everyday patient care, ensuring that treatment decisions are as personalized and effective as possible.
a. Potential Risks of Cannabis Use During Pregnancy
This summarizes illustrates that while there is evidence suggesting potential risks associated with prenatal cannabis exposure, many of these findings come from observational studies and are influenced by multiple overlapping factors. This complexity highlights the need for more nuanced research and individualized clinical assessments when considering cannabis use during pregnancy:
Impaired Placental Function: THC can cross the placenta and may disrupt its ability to deliver oxygen and nutrients by reducing blood flow and increasing permeability. This disruption could lead to nutrient deficiencies for the fetus. (Schreiber & Pick, 2019; Grant et al., 2018)
Low Birth Weight and Preterm Birth: Several observational studies have linked cannabis use during pregnancy to lower birth weight and an increased risk of premature delivery. However, these associations are often mixed with other factors, such as tobacco use or poor nutrition, making it difficult to pinpoint cannabis as the sole cause. (Corsi et al., 2019; Ryan et al., 2018)
Neurodevelopmental Alterations: Animal studies suggest that prenatal THC exposure can interfere with the normal development of the brain. By altering neurotransmitter systems—such as dopamine regulation—THC might affect the formation of neural connections, potentially leading to attention deficits, impulse control issues, or other cognitive challenges later in life. (Hurd et al., 2019)
Subtle Cognitive Impairments: Although gross structural birth defects have not been consistently linked to cannabis use, some research points to more subtle effects on cognitive functions such as learning, memory, and problem-solving abilities in later childhood. (Goldschmidt et al., 2008; Fried & Smith, 2001)
Behavioral Concerns: Longitudinal studies have noted that children exposed to cannabis in utero might exhibit mild behavioral differences, including increased impulsivity or difficulties with attention regulation. These findings are often small and influenced by additional factors, but they remain a concern for some researchers. (Fried & Smith, 2001)
Endocrine and Immune Function: Emerging evidence suggests that cannabis might affect hormonal balance and immune function during pregnancy, which could have downstream effects on fetal growth and development. However, this area requires further investigation to draw firm conclusions. (Costa, 2016)
Altered Placental Gene Expression: Some studies indicate that cannabis exposure could lead to changes in the way genes are expressed in the placenta. Such changes might influence how the placenta functions and, in turn, affect fetal development over the long term. (Trabucco et al., 2009)
Method-Dependent Risks: The way cannabis is consumed—whether by smoking, vaping, or using edibles—can significantly affect the amount and speed of THC absorption. For example, smoking may deliver high levels of THC quickly along with harmful byproducts like carbon monoxide, whereas edibles result in a slower onset of effects. These differences can lead to varying levels of fetal exposure, complicating our understanding of risk. (Grant et al., 2018)
Potential Impact on Fetal Cardiovascular Development: Preliminary studies suggest that cannabis exposure might affect fetal heart rate variability and overall cardiovascular development, although more research is needed to confirm these findings and understand their implications. (Gunn et al., 2016)
Individual Variability: Genetic differences among mothers can influence how they metabolize cannabinoids, meaning that one woman might have prolonged exposure to THC compared to another even if they consume similar amounts. This variability makes it even more challenging to predict the exact impact on fetal development. (Brik, 2024, Monfort-Ferré, 2022)
Variation in Use Patterns: Studies by Young-Wolff et al. (2019) show that cannabis use among pregnant women can vary widely—from daily use to only occasional use. These differences are important because more frequent use may carry higher risks, while sporadic use might be less harmful. This variation highlights the challenge of drawing broad conclusions about cannabis’s safety during pregnancy.
Challenges in Measuring Exposure: Research by El Marroun et al. (2011) found discrepancies between self-reported cannabis use and biochemical tests (such as urinalysis). This suggests that many pregnant women might underreport their cannabis consumption, making it difficult to accurately gauge how much exposure the fetus actually receives.
Compounding Effects of Multiple Risk Factors: Van Gelder et al. (2010) demonstrated that pregnant women who use cannabis often also face other risk factors, such as using other substances or living in challenging socioeconomic conditions. These overlapping influences make it hard to determine whether adverse outcomes like low birth weight are due solely to cannabis or a combination of factors.
The Need for an Integrated Approach: Forray (2016) emphasizes that focusing on cannabis in isolation may miss the broader picture of substance use during pregnancy. An integrated approach that considers all relevant factors—like concurrent use of tobacco or alcohol, stress levels, and nutrition—is crucial for understanding the overall impact on maternal and fetal health.
Long-Term Childhood Outcomes: Paul et al. (2023) examined the effects of prenatal cannabis exposure on children in a large-scale study. They found modest associations with later cognitive and behavioral outcomes, suggesting that while the risks might not be dramatic, there could be subtle long-term impacts that warrant further research.
Influence of Demographic Factors: Research by Young-Wolff et al. (2020) in a diverse cohort of pregnant women indicates that the adverse outcomes associated with cannabis use can be significantly influenced by demographic and social factors. This underscores the need for personalized risk assessments rather than one-size-fits-all recommendations.
Impaired Placental Function: Cannabis, particularly THC, can cross the placenta and may reduce blood flow or increase the "leakiness" of the placental barrier. This disruption can limit the transfer of oxygen and nutrients to the fetus, potentially leading to nutrient deficiencies. (Grant et al., 2018; Trabucco et al., 2009)
Low Birth Weight and Preterm Birth: Several observational studies have linked prenatal cannabis use with lower birth weight and an increased risk of premature delivery. However, many of these studies are complicated by other factors—such as tobacco use, poor nutrition, or high stress—that are already known to contribute to these outcomes, making it hard to pin the blame solely on cannabis. (Corsi et al., 2019; Ryan et al., 2018)
Neurodevelopmental Alterations: Animal studies suggest that prenatal THC exposure may disrupt normal brain development by interfering with processes like nerve cell migration and synapse formation. This interference can affect the regulation of neurotransmitters such as dopamine, which may lead to subtle cognitive or behavioral differences—such as issues with attention or impulse control—that could emerge later in life. (Hurd et al., 2019; Fried & Smith, 2001)
Subtle Cognitive and Behavioral Effects: Although major structural birth defects have not been consistently linked to cannabis use during pregnancy, some research indicates that children exposed to cannabis in utero might experience modest deficits in learning, memory, or problem-solving skills. These subtle differences may impact behavior, although they are often influenced by other factors as well. (Goldschmidt et al., 2008; Fried & Smith, 2001)
Method-Dependent Risks: The way cannabis is consumed can greatly influence how much THC reaches the fetus. For instance, smoking cannabis delivers THC rapidly and in high doses—along with harmful byproducts like carbon monoxide—while edibles result in slower, more prolonged exposure with lower peak levels. These variations can change the overall risk profile during pregnancy. (Grant et al., 2018)
Potential Impact on Fetal Cardiovascular Development: Some preliminary studies suggest that cannabis exposure might affect fetal heart rate variability and overall cardiovascular development. Although more research is needed, these effects could have important implications for the baby’s long-term health. (Gunn et al., 2016)
Variation in Use Patterns: Research has shown that cannabis use among pregnant women can range from occasional, low-dose use to daily, high-dose consumption. This wide variation makes it challenging to generalize the risks, as the potential impact on fetal development might differ substantially between light and heavy use.
(Young-Wolff et al., 2019)
Challenges in Measuring Exposure: Studies have found that self-reported cannabis use often does not match biochemical measurements, such as those obtained through urinalysis. This discrepancy can lead to underestimating the actual exposure of the fetus to THC, complicating the assessment of risk. (El Marroun et al., 2011)
Compounding Effects of Multiple Risk Factors: Many pregnant individuals who use cannabis also engage in other behaviors—such as smoking tobacco or consuming alcohol—or face socioeconomic challenges like high stress and poor nutrition. These factors are independently associated with adverse outcomes like low birth weight and premature birth, making it difficult to determine the specific contribution of cannabis.
(Van Gelder et al., 2010)
Integrated Approach and Long-Term Outcomes: An integrated approach that considers all these risk factors is essential for understanding the full impact of cannabis use during pregnancy. Long-term studies, such as those by Paul et al. (2023) and Young-Wolff et al. (2020), suggest that while adverse outcomes may be modest, subtle long-term impacts on cognitive and behavioral development could be present—though these effects are often intertwined with other influences.
b. Potential Benefits in Specific Clinical Scenarios
In cases where standard treatments fall short, cannabis may offer certain benefits during pregnancy. Although these potential benefits are still under investigation, many patients have reported improvements in various challenging situations. Here are several examples:
Relief for Severe Nausea:
For women experiencing severe hyperemesis gravidarum—characterized by constant, debilitating nausea that leads to dehydration and malnutrition—cannabis’s anti-nausea properties might help stabilize symptoms and prevent complications. By reducing the intensity of nausea, cannabis could help maintain proper hydration and nutritional intake, which are vital for both maternal and fetal health.
Chronic Pain Management:
Chronic pain conditions such as persistent back pain or fibromyalgia can be especially challenging during pregnancy, particularly when traditional pain relievers like opioids pose risks such as respiratory depression or neonatal withdrawal. Many patients report that cannabis provides effective relief from pain, allowing for improved mobility and a better quality of life without the severe side effects associated with other medications.
Mental Health Support:
Pregnancy can exacerbate mental health issues such as anxiety and depression. In situations where conventional antidepressants or anxiolytics are considered too risky or have not provided adequate relief, low-dose cannabis may help stabilize mood and improve sleep quality. This, in turn, can reduce stress and its harmful effects on both the mother and the developing baby.
Appetite Stimulation:
Severe nausea or other pregnancy-related symptoms can significantly diminish appetite, leading to nutritional deficiencies that affect fetal growth. Cannabis is known for its appetite-stimulating effects, which may help ensure that both mother and baby receive adequate nutrition during this critical period of development.
Anti-Inflammatory Effects:
Certain cannabis formulations—especially those high in CBD—have notable anti-inflammatory properties. These can help reduce inflammation-related discomfort or pain, offering an alternative for managing conditions where traditional anti-inflammatory drugs may not be safe during pregnancy.
Overall Stress Relief and Sleep Improvement:
Elevated stress and disrupted sleep are common during pregnancy and can have negative impacts on both maternal well-being and fetal development. Cannabis has been reported to help improve sleep quality and reduce anxiety, contributing to overall better health. Improved sleep and lower stress levels may, in turn, support a healthier environment for fetal growth.
These examples demonstrate how cannabis might provide relief in specific clinical scenarios where standard therapies do not work well. However, because each patient’s situation is unique, any decision regarding cannabis use during pregnancy should be made with careful clinical judgment and, ideally, under the guidance of a healthcare provider who is knowledgeable about the patient.
Think This Through: While cannabis may offer benefits for certain conditions during pregnancy—and many patients report positive effects—more rigorous research is essential to fully understand these benefits and to guide safe, personalized care. Individual differences play a critical role, affecting not only the mother’s well-being during this vulnerable time but also the developing fetus, whose growth during key periods can have lifelong implications.
c. Challenges with Existing Therapies and Why Some Turn to Cannabis
Many pregnancy-related conditions, such as severe nausea, chronic pain, and mental health disorders, are inadequately managed with conventional treatments, often despite multiple attempts with a wide range of treatment trials. For instance, first-line treatments for hyperemesis gravidarum (vitamin B6, doxylamine, ondansetron) may be ineffective or carry their own risks (e.g., potential teratogenicity). Similarly, standard treatments for anxiety and depression may lead to neonatal withdrawal symptoms or neurodevelopmental concerns. In these contexts, cannabis is sometimes viewed as the lesser risk by patients, who these days know many adults that consume without second guessing, and by doctors who have primarily learned about harms and risks in medical school, and are less familiar with the evidence on the other side of the scientific spectrum.
d. Risk-Benefit Balancing
In the absence of clear-cut evidence on either side, decisions about cannabis use during pregnancy must be highly individualized. Even though some peer-reviewed publications raise concerns about cannabis exposure, an equal number of rigorous studies have found no unambiguous evidence of harm. Nevertheless, major organizations—such as the American College of Obstetricians and Gynecologists (ACOG) and the Centers for Disease Control and Prevention (CDC)—continue to advise against cannabis use during pregnancy. They also acknowledge that difficult choices sometimes must be made when standard treatments fall short.
Providers and patients should work together through shared decision-making that takes into account several key factors: the severity of maternal symptoms and the risks of leaving them untreated; the dose, frequency, and method of cannabis use; the timing of exposure during pregnancy; and any additional risk factors, such as using other substances or facing socioeconomic challenges.
This approach calls for open and honest discussions in which healthcare providers admit that they might not have all the answers—especially with an issue as evolving as cannabis use during pregnancy—while patients are encouraged to ask thoughtful questions and share their personal experiences. By collaborating and learning from one another, both parties can navigate the complexities of cannabis use during pregnancy, ensuring that treatment decisions are as safe and tailored as possible.
Think This Through: When facing treatment decisions during pregnancy, how can one balance the immediate dangers of severe symptoms—such as debilitating nausea, pain, and stress—with the uncertain long-term effects that a treatment might have on fetal development? For example, if a mother is suffering from symptoms that could harm her and her baby right away, yet the potential risks of using a treatment like cannabis remain unclear over time, how should that balance be struck? Consider that the short-term benefits of relieving severe symptoms may be clear, but the long-term impacts on the baby are still not fully understood.
6. Cannabis & Pregnancy Frequently Asked Questions (FAQ) ❓
Does Cannabis Cause Birth Defects?
Current evidence does not show that cannabis use during pregnancy causes major structural birth defects like those seen with alcohol or drugs such as thalidomide. However, some animal studies suggest that prenatal THC exposure can subtly interfere with normal brain development—for example, by disrupting the migration of nerve cells and the formation of neural connections. These changes could potentially lead to minor differences in cognitive function or behavior later in life, though human studies have not consistently demonstrated significant neurodevelopmental deficits. More rigorous, long-term research is needed to determine whether these subtle changes have a meaningful impact on everyday life. (Hurd et al., 2019; Goldschmidt et al., 2008)
Is Cannabis Associated with Low Birth Weight and Preterm Birth?
Observational studies have noted a modest association between cannabis use during pregnancy and outcomes such as low birth weight and preterm birth. However, many women who use cannabis also face other well-known risk factors—such as tobacco smoking, alcohol use, poor nutrition, or high stress—which are known contributors to these outcomes. For instance, one study found that while cannabis use was linked to lower birth weight, the association became less clear when factors like tobacco use were accounted for. Similarly, research indicates that once lifestyle and socioeconomic factors are controlled for, isolating the independent effect of cannabis becomes challenging. Overall, while there appears to be a signal suggesting some risk, the true impact of cannabis on these outcomes is complex and influenced by multiple overlapping factors. (Corsi et al., 2019; Young-Wolff et al., 2020)
How Do THC and CBD Differ in Their Impact During Pregnancy?
THC is the psychoactive component in cannabis that readily crosses the placenta and may affect fetal brain development by interfering with the formation of neural connections. This interference could theoretically lead to subtle cognitive or behavioral changes in the child. In contrast, CBD does not produce a “high” and is known for its anti-inflammatory and potential neuroprotective benefits; however, research on CBD’s effects during pregnancy is extremely limited. Because most studies do not differentiate between THC and CBD, it remains unclear whether any adverse outcomes are due solely to THC or to a combination of cannabinoids. (Grant et al., 2018)
Can a Mother Safely Breastfeed If She Uses Cannabis?
THC is stored in fat tissues and can accumulate in breast milk, which means an infant may be exposed to THC for several weeks after birth. Although the long-term effects of this exposure are not fully understood, most professional organizations—including the American Academy of Pediatrics (AAP) and the Centers for Disease Control and Prevention (CDC)—advise against cannabis use during lactation. The primary concern is that even low levels of THC could potentially affect the developing brain of the infant. Until more definitive research is available, the safest approach is generally to avoid cannabis while breastfeeding. (Ryan et al., 2018)
What Do Major Medical Organizations Recommend Regarding Cannabis Use in Pregnancy?
Major health organizations such as the American College of Obstetricians and Gynecologists (ACOG), the CDC, the World Health Organization (WHO), and the AAP advise against the use of cannabis during pregnancy and breastfeeding. These recommendations are based on concerns about potential neurodevelopmental risks and the current lack of high-quality, conclusive evidence on cannabis’s safety in these contexts. Even though some studies report only subtle differences in outcomes, the prevailing guidance remains one of caution given the many unknowns surrounding cannabis’s impact on fetal development. (ACOG, CDC, WHO, AAP)
What Do Long-Term Studies Reveal About Children Exposed to Cannabis In Utero?
Long-term studies, including the Ottawa Prenatal Prospective Study, the Generation R Study, and the Maternal Health Practices and Child Development Study, have observed that children exposed to cannabis in the womb may exhibit subtle differences in attention, impulse control, and executive function. However, these outcomes are often influenced by additional factors such as maternal stress, nutrition, and socioeconomic status, making it difficult to determine the extent to which cannabis alone is responsible. While these findings suggest there might be a minor impact on neurodevelopment, the effects are generally modest, and further long-term research is needed to fully understand their significance. (El Marroun et al., 2011; Goldschmidt et al., 2008; Young-Wolff et al., 2020)
If I Used Cannabis Before Knowing I Was Pregnant, Should I Be Worried?
To an even-handed read of the full literature, occasional cannabis use before pregnancy is generally considered unlikely to cause major harm. Some studies suggest that women who cease using cannabis once they learn they are pregnant tend to have outcomes similar to those of non-users.
For example, Corsi et al. (2019) observed that adverse perinatal outcomes were less pronounced among women who discontinued cannabis use early in pregnancy compared to those who continued using it. Likewise, Young-Wolff et al. (2020) reported that women who ceased cannabis use had birth outcomes comparable to those of women who never used cannabis during pregnancy, highlighting the potential benefits of early cessation.
However, because each situation is unique, it is important for anyone with such a history to discuss it with their healthcare provider. This conversation can help determine whether additional monitoring or specific interventions are necessary to ensure the best possible outcome for both mother and baby.
Balancing Risks and Benefits
Think This Through: Imagine the decision-making process when standard treatments fail. A pregnant woman suffering from severe nausea or chronic pain might consider cannabis as an alternative option. In such a scenario, she must weigh the immediate dangers of untreated symptoms—such as dehydration or chronic stress—against the uncertain, subtle long-term effects that cannabis might have on her baby’s development. Additionally, within the realm of cannabis use, variations in dose, frequency, and consumption method can lead to different outcomes. These considerations underscore why personal and clinical judgment are so crucial in this area, as every pregnancy is unique and requires tailored, thoughtful care.
Bridging Research and Real-World Practice
Despite a growing body of research on cannabis use during pregnancy, many questions remain unanswered. Controlled studies attempt to minimize variables to isolate specific effects, but real-life pregnancies are much more complex. Factors such as genetics, stress, nutrition, and environmental exposures interact in ways that controlled experiments often cannot capture. As a result, healthcare providers frequently rely on their clinical experience and individualized judgment—especially when standard treatments fail—to tailor care to each patient’s unique situation. These real-world observations often reveal subtle patterns that have not yet been documented in academic research, emphasizing the importance of personalized care in managing the complexities of cannabis use during pregnancy.
Think This Through: Reflect on which FAQ speaks most to your concerns—whether it’s about birth defects, low birth weight, differences between THC and CBD, or another topic. For instance, if you’re particularly worried about how cannabis might affect your baby’s brain development, consider asking your provider, “Based on my health history and lifestyle, what do you think is the risk that cannabis could impact my baby’s brain development?” Or if low birth weight and premature birth worry you, you might ask, “How do my other factors—like nutrition or stress—affect these risks, and what alternatives could help manage my symptoms safely?” You could also inquire about the best strategies for stopping cannabis use if you have used it before knowing you were pregnant. By identifying your specific concerns and asking targeted questions, you can ensure that you receive personalized advice that takes your unique situation into account.
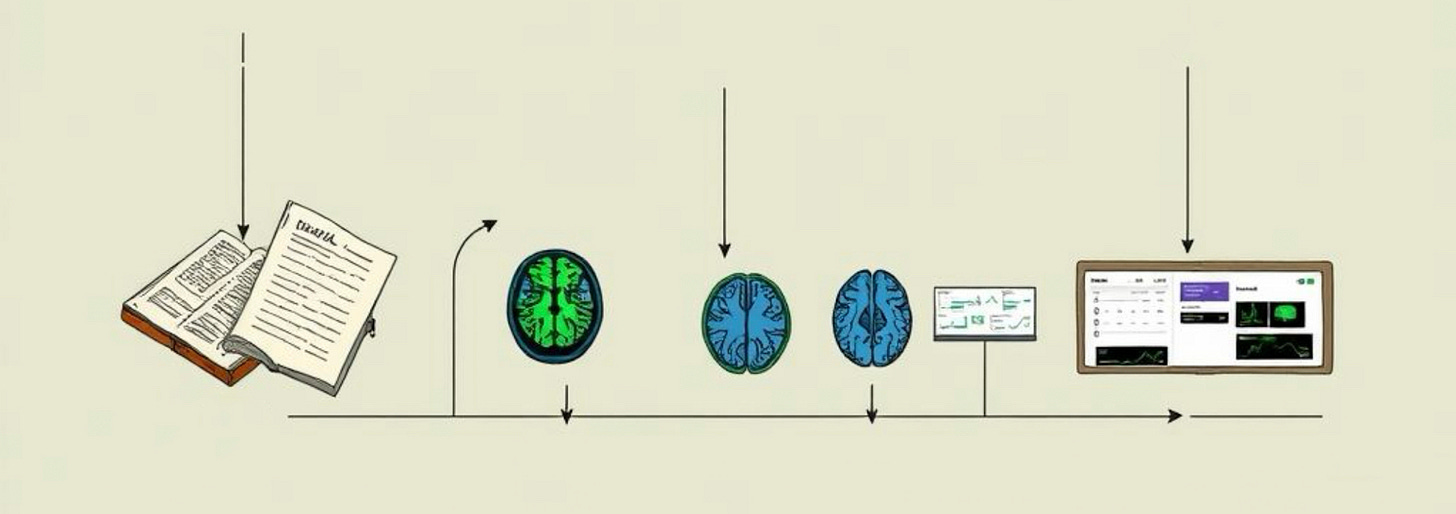
7. Historical Timeline and Key Research Findings ⏳
Research on prenatal cannabis exposure has evolved considerably over the past several decades, reflecting shifts in both scientific inquiry and cultural attitudes. Each era offers insights not only into the scientific findings but also into how medicine and society have viewed cannabis use during pregnancy.
1970s–1980s:
Early research focused primarily on basic birth outcomes—such as birth weight, prematurity, and overall neonatal health. Studies like the Ottawa Prenatal Prospective Study (initiated in 1978) tracked children exposed to cannabis and noted subtle differences in areas like attention and impulse control, even when IQ scores remained normal. Research by Fried et al. (1989) and Zuckerman et al. (1989) reported mild cognitive effects and slightly lower birth weights. However, these early studies were constrained by limited sample sizes, less rigorous controls, and a prevailing cultural stigma around cannabis use, which was widely associated with counterculture movements and strict legal prohibitions. This combination of factors meant that early research was both cautious and fragmented, reflecting the era’s conservative medical and societal attitudes. (Fried & Smith, 2001)
2000s–2010s:
As the medical and legal landscapes began to shift, larger cohort studies emerged that expanded the focus to include long-term neurodevelopmental outcomes and behavioral assessments. Studies like the Generation R Study in the Netherlands and the Maternal Health Practices and Child Development Study in the U.S. followed participants over many years, highlighting the significant influence of environmental and socioeconomic factors such as maternal stress, nutrition, and concurrent substance use. During this period, the cultural stigma around cannabis began to ease as more states legalized medical cannabis, leading to a more open debate. Nonetheless, researchers still faced challenges in disentangling cannabis’s effects from those of other risk factors. This era represents a transition toward more comprehensive research, although many questions remained unresolved. (Corsi et al., 2019; El Marroun et al., 2011)
2020s–Present:
Recent advances in technology and research methods—such as fetal brain imaging, epigenetic analyses, and genetic studies—have provided more detailed insights into how cannabis might affect fetal development at a molecular level. These cutting-edge techniques are beginning to uncover the complex interplay between cannabis dose, timing of exposure, and method of consumption. Culturally, the 2020s have seen further mainstream acceptance of cannabis, with many states fully legalizing its use for adults, which has in turn spurred more nuanced research. Despite these advances, clear cause-and-effect relationships remain elusive, and key questions persist regarding the long-term impact on both maternal and fetal health. This modern era illustrates the ongoing challenge of balancing sophisticated scientific findings with evolving cultural attitudes and clinical realities. (Young-Wolff et al., 2020; Paul et al., 2023)
Think This Through: How does understanding the evolution of research—from the early, cautious studies of the 1970s and 1980s, through the more expansive cohort studies of the 2000s and 2010s, to today’s advanced imaging and genetic research—shape your view of the current uncertainties and future directions in this field? Consider not only the scientific findings but also how cultural attitudes and changing medical practices have influenced our understanding of prenatal cannabis exposure.
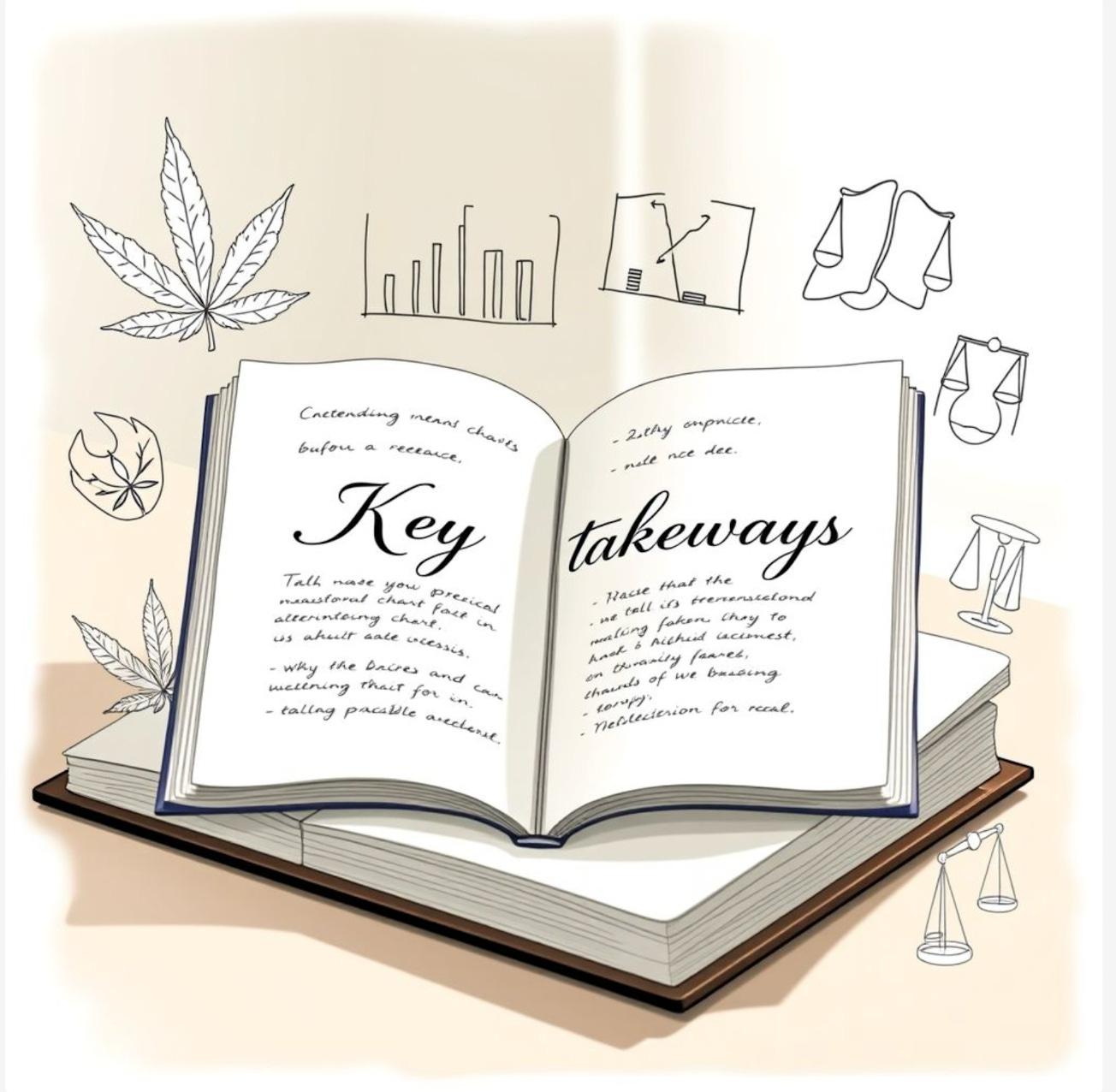
8. Key Takeaways and Recommendations 📝
The current state of knowledge regarding cannabis use during pregnancy is complex. On one hand, there are theoretical concerns that THC may disrupt key developmental processes through its interaction with the endocannabinoid system (ECS). On the other hand, epidemiological studies have not consistently demonstrated overt harm or defined a clear “cannabis syndrome.” Emerging hypotheses even suggest that for some mothers with naturally low levels of endocannabinoids, carefully managed cannabinoid supplementation might help restore balance—much like how vitamins can correct a deficiency. However, the research remains mixed and is complicated by confounding factors such as tobacco use, stress, and nutritional status. As a result, further rigorous, long-term studies are needed to clarify these effects.
Recommendations for Patients and Providers:
Engage in Open Communication:
Patients should have honest, in-depth discussions with a trusted provider who understands their unique health history. Providers should share all available evidence—even when it is inconclusive—to help guide decision-making.
Consider the Full Picture:
Treatment decisions should balance the potential benefits of alleviating severe symptoms (such as extreme nausea, chronic pain, or anxiety) with the uncertain long-term risks to fetal development. Recognize that factors like the dose, frequency, and method of cannabis use, as well as other personal risk factors, can all influence outcomes.
Personalize Care:
Given the complexity of the research and the numerous confounding variables, healthcare decisions regarding cannabis use must be highly individualized. This means tailoring treatment plans based on a mother’s baseline health, her specific symptoms, and her family and environmental context. It may also require plans to monitor the baby’s development over time.
Seek Expert Guidance:
In situations where standard treatments are ineffective, expert consultation can be invaluable. For cannabis-specific knowledge, telemedicine support from specialized clinics—like CED Clinic—can offer evidence-based insights to help manage the risks and benefits effectively.
Think This Through: Take a moment to reflect on the uncertainties surrounding cannabis use during pregnancy. On one hand, untreated severe symptoms—such as persistent nausea, chronic pain, or overwhelming stress—pose real and immediate risks to both mother and baby. On the other hand, the long-term effects of cannabis on fetal development remain unclear. Given that factors like genetics, lifestyle, and environmental exposures all play a part, it may be best to take a personalized approach. Working with a provider who knows your history can help balance these risks, ensuring that any treatment is tailored to your unique needs.
CED Clinic Experience:
At CED Clinic, hundreds of women have sought personalized counseling about their options regarding cannabis use during pregnancy and breastfeeding. The clinic’s experts understand that no two situations are alike, and that standard guidelines may not fit every case. By offering dedicated telemedicine support, CED Clinic is not only accessible at home, wherever that may be, but helps families navigate the complex balance between relieving severe symptoms and managing potential long-term risks. With an emphasis on ongoing follow-up, both the mother’s well-being and the baby’s development can be carefully monitored, and can help ensure that all of our patients receive the most current, evidence-based advice available.
Virtual Appointment (Learn More)
9. What The Future Holds for Research 🔮
The current evidence on cannabis use during pregnancy is far from complete, and many important questions remain unanswered. To better understand the risks and benefits, future research should focus on several key areas:
Longitudinal Studies:
Follow children exposed to cannabis in utero through adolescence and even into adulthood. This research would help assess lasting impacts on cognitive function, behavior, and physical health. Long-term tracking can reveal whether subtle neurodevelopmental differences observed in early childhood persist or evolve over time.
Dose-Response Relationships:
Precisely quantify the dose, frequency, and duration of cannabis use to differentiate between low, moderate, and high exposures. This kind of detailed data is essential to determine which levels of exposure might be safe and which could be harmful, providing clearer guidance for clinical practice.
Separation of Cannabinoid Effects:
Clearly distinguish between the effects of THC, CBD, and other cannabinoids. By isolating the impacts of each compound, researchers can determine if adverse outcomes are primarily due to THC, if CBD offers protective benefits, or if the combination of cannabinoids has a unique effect on both maternal and fetal health.
Advanced Imaging and Genetic Studies:
Utilize modern tools like fetal brain imaging and genetic/epigenetic analyses to unravel the mechanisms by which cannabinoids affect development. These techniques can provide a window into how cannabis interacts with the endocannabinoid system at a molecular level and help identify biomarkers of risk or benefit.
Addressing Polysubstance Use:
Design studies that can isolate the independent effects of cannabis from those of other substances, such as tobacco, alcohol, or prescription medications. Since many pregnant individuals who use cannabis also use other drugs, this research is crucial for understanding the true contribution of cannabis to any observed outcomes.
Investigating Maternal Endocannabinoid Deficiency:
Explore the prevalence and clinical significance of maternal endocannabinoid deficiency, and examine whether supplementing with cannabinoids can restore balance and support fetal development. This line of inquiry could reveal whether, in some cases, external cannabinoids might actually have therapeutic benefits rather than posing risks.
Think This Through: If future research were able to clearly define how different doses and types of cannabis affect pregnancy outcomes, and to separate the effects of THC from those of CBD. How might these findings change clinical guidelines? Would personalized care become the norm, with treatment plans tailored not only to a mother’s health history but also to her unique biological makeup? Or, would women feel more comfortable with self-care at home? As research uncovers more about the interplay between cannabis, the endocannabinoid system, and individual factors like genetics and lifestyle, healthcare providers might be able to offer more precise, evidence-based recommendations that better balance the immediate needs of the mother with the long-term health of the baby.
10. Case Studies and Vignettes 🎥
To bring these complex discussions into a real-world context, here are some anonymized case examples:
Case Study 1: Managing Hyperemesis Gravidarum
A 28-year-old pregnant patient experienced severe, persistent nausea in her first trimester—so intense that it led to repeated hospitalizations for dehydration and malnutrition. Standard anti-nausea medications provided little relief. After an in-depth discussion of the potential risks and benefits, she and her healthcare provider decided to try a low-dose cannabinoid regimen. With continuous telemedicine support from CED Clinic, her symptoms gradually improved. She was able to maintain proper hydration and nutrition, and her condition stabilized without any apparent adverse outcomes. This case illustrates how cannabis, when used under careful supervision, may offer relief when conventional treatments fail.
Case Study 2: Addressing Maternal Mental Health and Endocannabinoid Deficiency
A 32-year-old patient with a long history of depression and anxiety saw her symptoms worsen during pregnancy, even with conventional therapy. Emerging research on maternal endocannabinoid deficiency prompted her provider to consider low-dose CBD as an adjunct therapy. After a thorough evaluation and an open discussion about the potential benefits and uncertainties, her treatment plan was adjusted to include CBD. Over the ensuing weeks, her mood stabilized, her sleep improved, and she reported feeling more balanced overall. This case underscores the possibility that, for some women, cannabinoid therapy might help normalize an underactive endocannabinoid system—though it also highlights the need for careful, personalized monitoring.
Case Study 3: A Multimodal Approach to Chronic Pain
A pregnant patient suffering from chronic back pain, which had not responded well to standard non-opioid pain relievers, faced significant daily discomfort. Due to the known risks associated with opioid use during pregnancy, her healthcare provider suggested exploring alternative therapies. Together, they decided on a multimodal approach that included a low-dose cannabis tincture—chosen for its controlled dosing and avoidance of combustion-related toxins—along with physical therapy and lifestyle modifications. Over time, her pain levels decreased, allowing her to continue her daily activities with improved comfort. This case highlights how combining cannabis with other non-pharmacological interventions can create a balanced approach to pain management during pregnancy.
Think This Through:
Reflect on these case examples and consider the importance of individualized care. How do you think a personalized approach—one that takes into account a woman’s specific health history, current symptoms, and overall environment—can help navigate the uncertainties surrounding cannabis use during pregnancy? These cases demonstrate that when standard treatments fall short, a carefully tailored plan, supported by ongoing monitoring and expert guidance, can make all the difference in ensuring both maternal well-being and a healthy start for the baby.
11. Glossary of Terms 📖
Endocannabinoid System (ECS):
The ECS is a sophisticated biological system present in all vertebrates. It consists of receptors (primarily CB1 and CB2), endogenous ligands such as anandamide and 2-arachidonoylglycerol (2-AG), and the enzymes that synthesize and break down these molecules. This system plays a crucial role in regulating various physiological processes—including immune responses, mood, appetite, pain perception, neurodevelopment, and reproduction. In the context of pregnancy, the ECS is vital for proper implantation, placental development, and fetal brain formation, meaning any disruption to its normal function can potentially impact maternal and fetal health.
Teratogen:
A teratogen is any agent—be it a chemical, drug, virus, or environmental factor—that can interfere with normal embryonic or fetal development, potentially causing birth defects or malformations. Classic examples include certain prescription drugs (like thalidomide), alcohol, and some infections. The study of teratogens helps healthcare providers understand which exposures during pregnancy can lead to developmental abnormalities and guide them in advising expectant mothers.
Hyperemesis Gravidarum (HG):
Hyperemesis gravidarum is a severe form of nausea and vomiting during pregnancy that goes beyond typical “morning sickness.” It can lead to significant dehydration, electrolyte imbalances, and weight loss, sometimes requiring hospitalization. Unlike common nausea, HG can have a profound impact on both maternal health and fetal development if left untreated. The condition often necessitates careful medical management and sometimes prompts patients to explore alternative treatments, including the use of cannabis for symptom relief.
Cannabinoids:
Cannabinoids are a class of chemical compounds that interact with the body’s ECS. The most well-known cannabinoids include THC (tetrahydrocannabinol) and CBD (cannabidiol). THC is responsible for the psychoactive effects of cannabis, meaning it can alter perception, mood, and behavior by binding to CB1 receptors in the brain. CBD, on the other hand, does not produce a “high” and is thought to have various therapeutic properties, such as anti-inflammatory and anti-anxiety effects. Research into cannabinoids is ongoing, with particular attention paid to how these compounds may affect different aspects of health, including during pregnancy.
Cannabis Addiction vs. Cannabis Dependence:
Cannabis Addiction refers to a behavioral pattern characterized by compulsive use, a loss of control over consumption, and continued use despite clear adverse consequences on personal, social, or occupational functioning.
Cannabis Dependence describes a physiological or psychological adaptation to regular cannabis use, which may include tolerance (needing higher doses to achieve the same effect) and withdrawal symptoms upon cessation. Importantly, dependence can sometimes occur in a therapeutic context where cannabis is used to manage symptoms without leading to the dysfunction or disability typically associated with addiction.
Non-Smoked Cannabis Delivery Methods:
This term encompasses various forms of cannabis consumption that do not involve smoking. Common non-smoked methods include:
Edibles: Cannabis-infused food or beverages that are ingested, offering a slower onset of effects with a longer duration compared to inhaled forms.
Tinctures: Liquid extracts made by dissolving cannabis compounds in alcohol or oil, typically administered under the tongue (sublingually) for relatively rapid absorption without the harmful byproducts of combustion.
Capsules: Pills containing measured doses of cannabis extracts, offering precise dosing in a convenient format.
Topicals: Creams, balms, or lotions infused with cannabis that are applied directly to the skin to provide localized relief, such as reducing inflammation or pain, without significant systemic absorption.
Non-Altering Cannabinoids:
These are cannabinoid compounds—such as CBD (cannabidiol)—that do not produce the intoxicating “high” typically associated with cannabis. They may offer therapeutic benefits like reducing inflammation, easing anxiety, or improving sleep quality without altering mental state. This characteristic makes them particularly attractive for individuals seeking medicinal relief without impairment.
Topicals (Cannabis-Infused Topicals):
Topicals are cannabis-infused products (e.g., creams, balms, gels) applied directly to the skin. They are designed to target localized issues such as joint pain, muscle soreness, or skin conditions. Because topicals are intended for local application, they generally produce minimal systemic absorption, meaning they are unlikely to result in psychoactive effects. This makes them an appealing option for patients who want the benefits of cannabis without the risk of systemic intoxication.
Placental Efficiency:
Placental efficiency refers to the effectiveness of the placenta in transferring essential nutrients and oxygen from the mother to the developing fetus. A highly efficient placenta supports healthy fetal growth and development, while reduced efficiency can be linked to complications such as low birth weight, preterm birth, or other developmental issues. Researchers study placental efficiency to understand how various exposures (including potential toxins or drugs) might impact fetal health.
Polysubstance Use:
Polysubstance use describes the concurrent consumption of more than one substance, such as cannabis, tobacco, and alcohol. This phenomenon is significant in research and clinical practice because the effects of one substance can interact with or mask the effects of another, complicating the assessment of individual risks. For instance, when studying the impact of cannabis on pregnancy, it is essential to account for the fact that many users might also be exposed to other substances that independently influence fetal development and pregnancy outcomes.
12. Linked Full PDFs of References & Sources 📚
The following list of references are a collection drawn from peer-reviewed journals, meta-analyses, and high-quality observational studies to support the discussion in this document. Links to free PDFs are provided for every reference, for those who want to read the primary literature.
In addition to the links below, here is an additional folder of 111 studies on this topic of cannabis and pregnancy for all who want to read more, free of costs. 📚 🤯
Torres, C. A., Medina-Kirchner, C., O’Malley, K. Y., & Hart, C. L. (2020).
Totality of the evidence suggests prenatal cannabis exposure does not lead to cognitive impairments: A systematic and critical review. Frontiers in Psychology, 11, 816.American College of Obstetricians and Gynecologists (ACOG). (2017). Marijuana Use During Pregnancy and Lactation. Committee Opinion No. 722.
Paul, S. E., Hatoum, A. S., Fine, J. D., Johnson, E. C., Hansen, I., Karcher, N. R., & Bogdan, R. (2023). Associations Between Prenatal Cannabis Exposure and Childhood Outcomes: Results From the ABCD Study. JAMA Network Open, 6(3), e225822.
Schreiber, S., & Pick, C. G. (2019). Cannabis and Pregnancy—Towards Better Understanding of the Implications. International Journal of Molecular Sciences, 20(19), 5091.
Gunn, J. K. L., Rosales, C. B., Center, K. E., Nuñez, A., Gibson, S. J., Christ, C., & Ehiri, J. E. (2016). Prenatal exposure to cannabis and maternal and child health outcomes: A systematic review and meta-analysis. BMJ Open, 6(4), e009986.
Ryan, S. A., Ammerman, S. D., & O’Connor, M. E. (2018). Marijuana Use During Pregnancy and Breastfeeding: Implications for Neonatal and Childhood Outcomes. Pediatrics, 142(3), e20181889
Hurd, Y. L., Wang, X., Anderson, V., Beck, O., Minkoff, H., & Dow-Edwards, D. (2019). Cannabis Use and Neural Development: Findings From Longitudinal Studies and Animal Models. Neuropsychopharmacology, 44(1), 211–222.
Westfall, R. E., Janssen, P. A., Lucas, P., & Capler, R. (2006). Survey of medicinal cannabis use among childbearing women: Patterns of use and potential harm. Complementary Therapies in Clinical Practice, 12(1), 27–33.
Corsi, D. J., Hsu, H., El-Chaar, D., et al. (2019). Association Between Self-reported Prenatal Cannabis Use and Maternal, Perinatal, and Neonatal Outcomes. JAMA, 322(2), 145–152.
Grant, K. S., Petroff, R., Isoherranen, N., Stella, N., & Vauzour, D. (2018). Cannabis Use during Pregnancy: Pharmacokinetics and Effects on Child Development. Pharmacology & Therapeutics, 182, 133–151.
Costa, M. A. (2016). The Endocannabinoid System: A Novel Player in Human Placental Development. Journal of Clinical Endocrinology & Metabolism, 101(2), 447–457.
Taylor, A. H., Bachkangi, P., & Konje, J. C. (2023). Labour and premature delivery differentially affect the expression of the endocannabinoid system in the human placenta.
Histochemistry and Cell Biology, 160(5), 577–593.Sun, X., & Dey, S. K. (2012). Endocannabinoid signaling in female reproduction. ACS Chemical Neuroscience, 3(5), 349–355..
Melford, S. E., Taylor, A. H., & Konje, J. C. (2021). Nitric oxide positively affects endometrial receptivity via FAAH and NAPE-PLD in vitro.
Reproduction and Fertility, 2, 107–116.Fonseca, B. M., Correia-da-Silva, G., & Teixeira, N. A. (2013). Cannabinoid-induced cell death in endometrial cancer cells: Involvement of TRPV1 receptors in apoptosis. Journal of Physiology and Biochemistry, 69(2), 321–332.
Maia J, Almada M, Silva A, Correia-da-Silva G, Teixeira N, Sá SI, Fonseca BM. The endocannabinoid system expression in the female reproductive tract is modulated by estrogen. J Steroid Biochem Mol Biol. 2017 Nov;174:40-47.
Karasu, T., Marczylo, T. H., Maccarrone, M., & Konje, J. C. (2011). The role of sex steroid hormones, cytokines and the endocannabinoid system in female fertility. Human Reproduction Update, 17(3), 347–361.
Trabucco, E., Acone, G., Marenna, A., et al. (2009). Endocannabinoid system in first trimester placenta: Low FAAH and high CB1 expression characterize spontaneous miscarriage. Placenta, 30(6), 516–522.
Habayeb, O. M., Taylor, A. H., Bell, S. C., et al. (2008). Expression of the endocannabinoid system in human first trimester placenta and its role in trophoblast proliferation. Endocrinology, 149(10), 5052–5060.
Wang H, Xie H, Dey SK. Endocannabinoid signaling directs periimplantation events. AAPS J. 2006;8(2):E425-32.
Fried, P. A., & Smith, A. M. (2001). Neurotoxicology and Teratology, 23(1), 1–11.
Avalos, L. A., Oberman, B., Alexeeff, S., et al. (2024). Early Maternal Prenatal Cannabis Use and Child Developmental Delays. JAMA Network Open, 4(10), e2129102.
Goldschmidt, L., Richardson, G. A., Willford, J., et al. (2008). Prenatal Marijuana Exposure and Intelligence Test Performance at Age 6. JAMA Pediatrics, 162(6), 530–537.
Taneja, S., Panday, J., Popoola, A., et al. (2023). Making Informed Choices About Cannabis Use During Pregnancy and Lactation: A Qualitative Study of Information Use. Birth, 50, 504–512.
Ko, G. D., Bober, S. L., Mindra, S., & Moreau, J. M. (2016). Medical cannabis – The Canadian perspective. Journal of Pain Research, 9, 735–744.
Babson, K. A., Sottile, J., & Morabito, D. (2017). Cannabis, cannabinoids, and sleep: A review of the literature. Current Psychiatry Reports, 19(4), 23. doi:10.1007/s11920-017-0775-9
Rodondi, N., Pletcher, M. J., Liu, K., Hulley, S. B., & Sidney, S. (2006). Association between marijuana use and body mass index in young adults. American Journal of Medicine, 119(7), 1–6. doi:10.1016/j.amjmed.2005.08.046
Torres, C. A., Medina-Kirchner, C., O’Malley, K. Y., & Hart, C. L. (2020). Totality of the Evidence Suggests Prenatal Cannabis Exposure Does Not Lead to Cognitive Impairments: A Systematic and Critical Review. Frontiers in Psychology, 11, 816
13. The Executive Summary: Cannabis Use During Pregnancy
This document shares a gold standard overview of the current state of knowledge regarding cannabis use during pregnancy as of 2025. It synthesizes the latest findings, acknowledges the complexity of the research, and outlines practical considerations for both patients and healthcare providers.
Rising Prevalence: Cannabis use among pregnant individuals has increased significantly over the past decade. Self-reported use has risen from approximately 3.4% in 2002 to around 7.0% in more recent years, reflecting both changing legal landscapes and evolving cultural attitudes.
Research Challenges: The field faces major obstacles, including a lack of randomized controlled trials and difficulties in separating the effects of cannabis from confounding variables (such as tobacco use, stress, and nutrition). Moreover, many studies struggle to differentiate between the impacts of THC—the psychoactive component—and CBD, which is non-intoxicating but less well studied.
Key Concerns:
Fetal Development: THC is known to cross the placenta and may interfere with fetal brain development by disrupting neural connectivity.
Placental Function: Cannabis use may alter placental blood flow and increase its permeability, potentially affecting nutrient and oxygen delivery to the fetus.
Birth Outcomes: Some observational studies have linked cannabis use with low birth weight and preterm birth; however, these associations are often complicated by other risk factors.
Potential Benefits: In cases where standard treatments fall short—such as severe hyperemesis gravidarum, chronic pain conditions, or significant mental health challenges—cannabis may offer therapeutic benefits. Anecdotal and preliminary evidence suggests it might provide relief in these specific clinical scenarios, although more targeted research is needed.
Inconsistent Findings: Recent studies have produced conflicting results. Some research indicates potential risks at birth and subtle long-term neurodevelopmental impacts, while other studies find no clear, significant harm. This inconsistency underscores the complexity of the subject.
The Endocannabinoid System (ECS): The body’s natural ECS plays a crucial role in pregnancy—from aiding implantation to supporting fetal brain development. Its interaction with plant-based cannabinoids further complicates our understanding, highlighting the need for more research on both the risks and potential benefits.
Decision-Making: Given the complex and sometimes contradictory evidence, healthcare decisions regarding cannabis use during pregnancy must be highly individualized. Providers and patients should engage in shared decision-making that balances the potential benefits of alleviating severe symptoms against the uncertain long-term risks for the fetus.
Future Research: Priorities include conducting longitudinal studies that follow children exposed in utero into adolescence and adulthood, refining dose-response analyses, and clearly distinguishing the effects of THC, CBD, and other cannabinoids. Additionally, research should focus on different consumption methods and better control for confounding factors to provide clearer, evidence-based guidance.
This summary underscores that while significant progress has been made in understanding prenatal cannabis exposure, many uncertainties remain. As research continues to evolve, individualized clinical care—supported by open dialogue between patients and trusted providers—remains essential for safely navigating these complex issues.
Resources to Learn More:
Women’s Health & Hormonal Conditions