Cannabis as a Potential Solution for Metabolic Syndrome
Groundbreaking New Study Unveils the Metabolic Benefits of Cannabis Use
Metabolic Syndrome:
Metabolic syndrome is a collection of health issues like high blood pressure, high blood sugar, excessive fat around the waist, and abnormal cholesterol levels. When these conditions occur together, the combination increases the risk of serious conditions like heart disease, stroke, and type 2 diabetes.
Obesity Epidemic
Worldwide, obesity has become an inescapable health crisis affecting individuals across all age groups and demographics. Among children and adolescents, obesity rates have tripled over the past three decades, with one in five school-aged children in the United States now classified as obese, leading to an alarming rise in related health issues such as type 2 diabetes and hypertension. Adults are not spared either, with nearly 40% of the adult population in the United States classified as obese, contributing to increased risks of cardiovascular diseases and certain cancers. Even the elderly are increasingly affected, as excess weight worsens nearly all age-related conditions like osteoarthritis and decreases overall mobility and quality of life.
Ozempic, Wegovy, Monjaro, Victoza, Saxenda, Rybelsus, etc
In the midst of this growing epidemic of obesity and metabolic syndrome (MetS), finding effective treatments and management strategies is more critical than ever. Traditional approaches involving lifestyle modifications and pharmacological interventions have shown some success, but they are not universally accessible and certainly don’t work for everyone. The latest craze sweeping the world is the use of GLP-1 inhibitors (Ozempic, Wegovy, Monjaro, Victoza, Saxenda, Rybelsus, etc.), where the promise of weight loss, at least, seems “accessible,” although expensive, and the jury is still out on any long-term impacts.
Cannabis: Really? Yes!
Emerging research suggests that cannabis, a plant with a complex history and diverse effects, might offer a novel avenue for managing Metabolic Syndrome. A recent study, Prevalence of Metabolic Syndrome Among Emerging Adult Cannabis Users by Race/Ethnicity- Analysis of the 2009-2018 National Health and Nutrition Examination Surveys, focuses on the relationship between cannabis use and Metabolic Syndrome in young adults. This recent work presents some amazing findings that could reshape our understanding of metabolic health.
Significance of the Study
This study represents a leap in understanding just how meaningfully cannabis might influence metabolic health. Conducted using data from the National Health and Nutrition Examination Survey (NHANES) from 2009 to 2018, the research focused on individuals aged 18-25, a group with the highest prevalence of cannabis use. The findings suggest that cannabis users have a 42% lower prevalence of Metabolic Syndrome compared to non-users. For non-Hispanic Black (NHB) individuals, the reduction is even more significant, with cannabis users having a 78% lower prevalence of MetS.
These staggering results highlight the amazing potential of cannabis to positively impact metabolic health, especially in populations that are disproportionately affected by metabolic syndrome. The study found that cannabis use is associated with improved HDL cholesterol levels and healthier body composition, evidenced by lower body mass index (BMI) and waist circumference. This is particularly noteworthy in a public health landscape where obesity and metabolic disorders are rampant.
For subscribers: scroll down for a list of the cannabinoids benefits on obesity, lipid levels, insulin sensitivity, inflammation, and cardiovascular health.
Applicability and Broader Implications
The relevance of these findings extends beyond this immediate study population of 18-25 year olds. For many, especially those with limited access to traditional healthcare options (or limited funds), cannabis suddenly presents a potential alternative for managing aspects of metabolic health, and in a way that’s actually pleasant and an enjoyable of the day. The study’s findings indicate that cannabis might be incorporated into wider public health strategies to address MetS, as long as this approach is pursued with caution given the study’s limitations.
One of the most significant implications of this study is the potential for cannabis to serve as a complementary therapy. The traditional treatments for metabolic syndrome (stringent lifestyle changes and medications), many not be sustainable for everyone, and in some cases, they are hardly even feasible (costs, routines, accessibility). Cannabis, with its ability to interact with the endocannabinoid system (ECS) and regulate metabolism, appetite, and inflammation, offers a unique and potentially more accessible alternative.
Study Limitations and Unspoken Considerations
While the study’s findings are promising, it’s crucial to recognize its limitations. Science demands a balanced perspective, evaluating reported benefits and concerns in the context of the specific population studied. For instance, this study’s cross-sectional design can only establish associations, not causality. This leaves open questions about the direction of the relationship between cannabis use and metabolic syndrome. Does cannabis use reduce the risk of MetS, or are individuals with a lower risk of MetS more likely to use cannabis?
In a world saturated with stories linking cannabis to psychosis, mood disorders, or other sensational fears, it’s essential to remember that these are associations, not definitive proof of causation. Despite the appeal of such demonizing narratives to those who oppose cannabis, they remain speculative connections, much like the positive associations found in this study. The true relationship between cannabis and metabolic syndrome, as with any such association, requires further research to understand the big picture, which until very recently, has been a giant image missing consideration of one the most influential physiologic systems in the human body: the endocannabinoid system.
The reliance, in this study, on self-reported data for cannabis use introduces the possibility of recall and social desirability biases. Participants may not accurately report their cannabis consumption, leading to potential misclassification. Moreover, the study lacks detailed information on cannabis use patterns, such as the specific strains, THC and CBD content, and methods of consumption. These factors could significantly influence metabolic outcomes but were not captured in the research.
The inclusion of pregnant women without specific exclusion or adjustment introduces another layer of variability. Pregnancy significantly impacts metabolism, and including pregnant participants without accounting for this could skew the results. Additionally, the study does not fully account for critical factors like dietary habits, physical activity, and genetic predispositions, which play significant roles in metabolic health. There is nothing about this study which excludes such factors in an outlandish way, relative to the non-cannabis literature, but they are concerns for consideration, nevertheless.
Context in the Greater Public Health Landscape
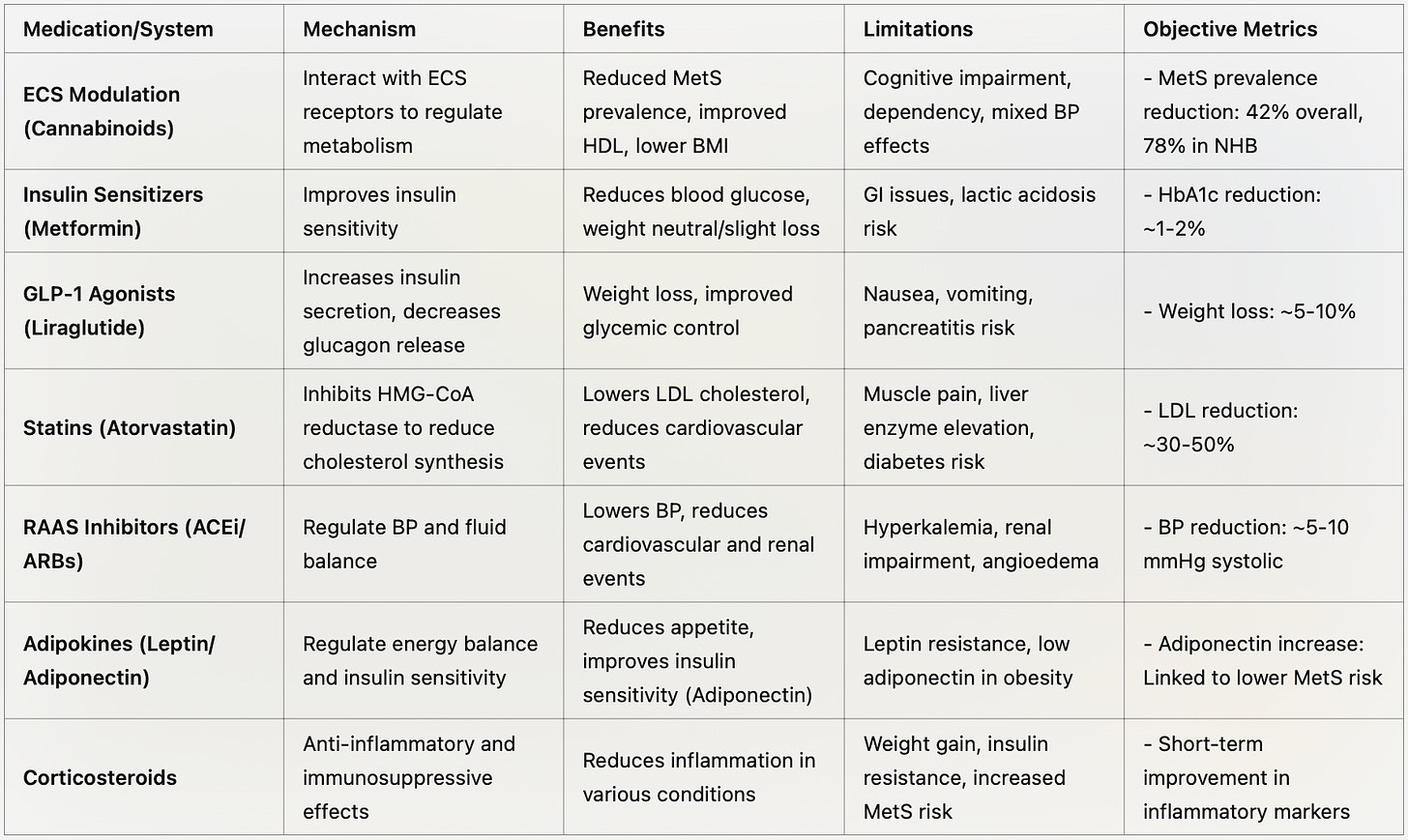
In the context of an obesity epidemic and the increasing prevalence of metabolic syndrome, this study highlights the importance of exploring alternative and complementary therapies. Cannabis has unique interactions with the ECS, this complex system that plays a crucial role in regulating energy balance, appetite, and inflammation, and yet is nearly fully absent from medical education or consideration. The study’s findings suggest that cannabinoids like THC and CBD might positively impact these processes, offering benefits such as reduced prevalence of MetS, improved HDL cholesterol levels, and healthier body composition. If not cannabis, it’s business as usual with existing options like insulin sensitizers, GLP-1 agonists, statins, and rigorous lifestyle modifications. While these traditional treatments are effective for many, they often come with accessibility issues and side effects, underscoring the need for exploring alternative therapies like cannabis.
Future Directions and Public Health Strategies
Until the medical establishment updates its education to include comprehensive information on the endocannabinoid system, patients need to consider a holistic approach to managing metabolic syndrome. This means integrating the endocannabinoid system with traditional methods. Personalized medicine that accounts for individual responses to cannabis, along with lifestyle interventions and thorough patient education, will be crucial for addressing complex cases. Simpler solutions will emerge for less complex cases. Moving forward, further research will likely focus on identifying which components of cannabis contribute to these metabolic benefits and understanding how they work.
Public health policies deserve to find a place on the cultural roadmap for a tune-up too. Policies must be informed by a nuanced understanding of cannabis’s benefits and risks. As legalization approaches and acceptance of cannabis continue to grow, ensuring safe and informed use is paramount. This study adds a valuable piece to the puzzle but underscores the need for continued research and dialogue among healthcare providers, policymakers, and the public.
Take Aways
This study sheds light on the potential of cannabis to influence powerful aspects of metabolic health, particularly in the context of an escalating public health crisis marked by rising obesity and metabolic syndrome. While the findings are promising, as with all science, they must be read within the context of the study’s limitations. Next stage research, particularly longitudinal studies and randomized controlled trials, is essential to establish causality and understand the long-term effects of cannabis on metabolic health, but these are strong effects that must not be overlooked.
As we continue to explore the potential of cannabis as a complementary therapy for metabolic syndrome, a holistic and evidence-based approach will help the medical industry appreciate the influence and opportunity of cannabinoid-based therapies. By integrating cannabis with traditional treatments and considering the diverse needs and responses of different populations, we can develop more effective and inclusive strategies for managing metabolic health. This study represents an important step in that direction, offering new hope and possibilities in the fight against metabolic syndrome and the ravages of the obesity epidemic.
Bonus: what might this mean for the health of our culture, big picture?
also, see below for a chart version of “Benefits of Cannabis on Metabolic Syndrome,” “Cannabis Compared to Other Metabolic Controllers,” a summary of “The Significant Results from this Study, Study images, and a list of 25+ studies that support similar findings, with links to each paper.
Keep reading with a 7-day free trial
Subscribe to Doctor-Approved Cannabis to keep reading this post and get 7 days of free access to the full post archives.